Unmasking Silent Threats: 7 Lacunar Stroke Warning Signs for Seniors (The #4 Symptom Most People Miss)
Lacunar strokes, often referred to as “silent strokes,” frequently go undetected in adults over 60. Unlike their larger counterparts, these small vessel events subtly disrupt brain function, progressively impacting mobility, cognitive abilities, and overall independence. Many individuals mistakenly attribute these gradual, often overlooked changes to the normal aging process. Intriguingly, medical imaging reveals that silent lacunar infarcts are present in the MRI scans of 20-30% of seemingly healthy older adults, with this prevalence rising significantly after age 80. Recognizing these understated indicators can be crucial for initiating timely discussions with a healthcare provider about vascular health. Continue reading—we’ll soon delve into a specific sign so commonly dismissed as simply “getting older” that it often prevents individuals from seeking vital medical evaluation, despite its potential to signal significant underlying brain changes.
Why Lacunar Strokes Are Particularly Dangerous and Frequently Missed
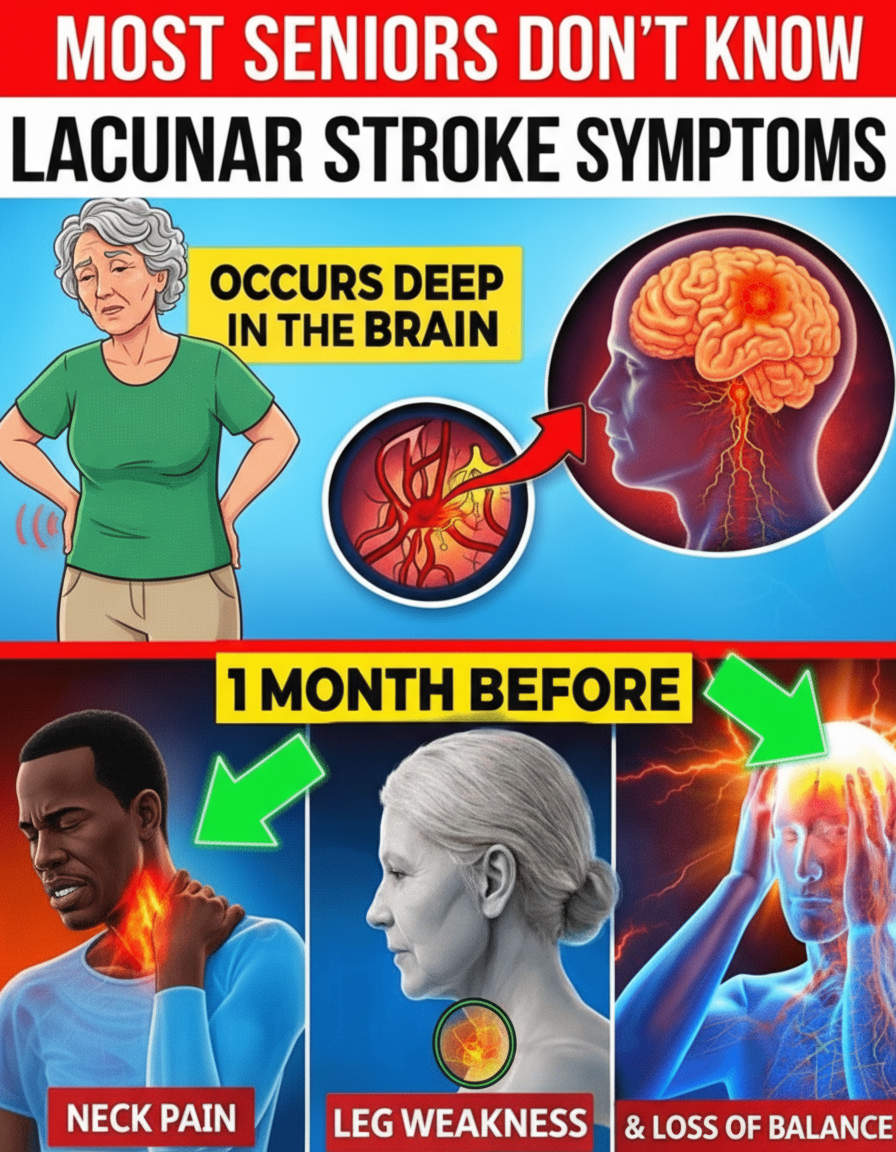
Lacunar strokes occur when minute penetrating arteries deep within the brain become obstructed, typically due to chronic conditions such as uncontrolled high blood pressure or the accumulation of cholesterol (atherosclerosis). These tiny vessels, often merely 0.2 to 0.8 mm in diameter, lead to localized damage that forms small cavities, or lacunae, in critical areas like the basal ganglia, thalamus, or white matter tracts. A significant majority of these incidents (up to 70-80%) initially produce no discernible symptoms, allowing daily routines to continue uninterrupted. However, over a span of years, recurrent micro-infarcts can accumulate, eventually reaching a threshold where noticeable impairments emerge in movement, sensation, balance, bladder control, and cognitive function. Research consistently demonstrates that these strokes elevate the risk of future cerebrovascular events, accelerate cognitive decline, and diminish a person’s ability to live independently. The encouraging news is that proactive management of key vascular risk factors—such as maintaining healthy blood pressure levels—can effectively slow the progression of damage when addressed early. Yet, the primary challenge remains: identifying these subtle warning signs before they escalate into more severe health complications.
The 7 Subtle Warning Signs of Lacunar Strokes that are Often Overlooked
These distinct patterns are derived from extensive clinical observations and findings published in leading neurology journals. They possess characteristics specific enough to differentiate them from general age-related changes when examined closely.
Warning Sign #7: Sudden, Intense, Unilateral Sensory Disturbances (Sharp, Stabbing, or Burning Pain)
Imagine experiencing an abrupt, severe burning, stabbing, or electric-shock sensation in a specific area like your hand, foot, or face—crucially, often localized to just one side of the body—without any apparent injury or clear cause. This can also manifest as extreme hypersensitivity, where even a light touch feels agonizing. Such symptoms may indicate damage within the thalamus, the brain’s vital sensory relay center. This type of central neuropathic pain can be persistent and challenging to manage, sometimes appearing suddenly following a small vessel occlusion. If you encounter sudden, one-sided, and unusual sensory experiences, it is imperative to discuss them promptly with a healthcare professional.
Warning Sign #6: Unexplained Severe Abdominal or Flank Pain
In rare instances, individuals might report intense, wave-like cramping or significant discomfort in the abdomen or side, symptoms that can mimic conditions like kidney stones or other gastrointestinal issues. However, despite thorough medical examinations, no physical cause is found. This atypical presentation may arise from disrupted pain signaling pathways located in deeper brain structures. When conventional diagnostic tests yield negative results, exploring the possibility of underlying cerebrovascular health issues becomes a relevant next step.
Warning Sign #5: Transient or Mild Weakness or Clumsiness in One Limb
A sudden feeling of heaviness, inadvertently dropping objects, or uncharacteristic clumsiness in one arm or leg—even if these symptoms last only a few minutes or hours—can be a critical indicator. These are often categorized as pure motor symptoms, typically affecting regions like the internal capsule or pons. While these episodes might resolve quickly (similar to a transient ischemic attack, or TIA), they serve as a potent warning sign for the risk of more permanent neurological changes if left unaddressed. Even minor or temporary weakness warrants immediate medical attention; never assume it’s merely a result of fatigue or overexertion. Consider a brief self-assessment: Have you recently noticed one-sided weakness or a tendency to drop things? Do these symptoms appear intermittently? How long have they been occurring?
Warning Sign #4: Progressive Difficulty with Balance, Gait, and Unexplained Falls (The One Everyone Overlooks)
This particular symptom is arguably the most frequently dismissed: a gradual onset of shuffling steps, a sensation of feet being “stuck” to the floor, requiring numerous small steps to turn, momentary freezing during movement, or recurrent, unexplained stumbles. When linked to multiple lacunar changes in the basal ganglia or white matter, this presentation is often termed vascular parkinsonism. It predominantly affects the lower body and typically lacks the tremor characteristic of classic Parkinson’s disease. Research in movement disorder studies indicates that up to 30% of parkinsonism cases in older adults have a vascular origin, and these often respond poorly to standard Parkinson’s medications. Family members are frequently the first to observe these changes, noticing that loved ones appear unsteady or hesitant in their movements. Many people incorrectly attribute these issues to arthritis or simply “getting old,” leading to significant delays in seeking proper medical evaluation. Take a moment to reflect: have you or a loved one noticed these subtle but persistent changes in mobility?