Those small, persistent white bumps on your face—often around the eyes, cheeks, or forehead—can be incredibly frustrating, especially when they linger for months and refuse to budge no matter how much you cleanse or exfoliate. Many people mistake them for acne and try popping or harsh scrubbing, only to end up with irritation, redness, or even scarring that makes the skin look worse. The truth is, these aren’t pimples at all; they’re milia, tiny keratin-filled cysts that form under the skin’s surface, and treating them like acne can do more harm than good.
But here’s the good news: with the right gentle, evidence-based approach, you can help prevent new ones, encourage gradual improvement in skin texture, and restore a smoother, more even appearance. Stick around—by the end, you’ll discover a simple daily plan that dermatologists often recommend for lasting clarity, plus why some popular DIY trends might be holding you back.

The Common Confusion: Why Those White Bumps Aren’t Acne (And Why It Matters)
Milia and acne may look similar at first glance—both can appear as small white spots—but they’re fundamentally different. Acne involves clogged pores filled with oil, bacteria, and inflammation, often leading to redness, swelling, or pus. Milia, on the other hand, are small cysts formed when keratin (a natural skin protein) gets trapped beneath the surface as dead skin cells fail to shed properly.
This distinction matters because acne treatments like harsh scrubs or pore-stripping products can irritate milia-prone skin and potentially worsen the issue. Studies and dermatologist insights show that milia are harmless and non-inflammatory, but forcing them out risks damage, infection, or scarring—something no one wants when aiming for clearer skin.
Research from sources like the Cleveland Clinic highlights that milia affect people of all ages, though they’re especially common in adults dealing with skin changes over time.

Milia Explained: Causes, Types, and Why They Appear Around Eyes and Face
Milia form when dead skin cells and keratin become trapped under the epidermis, hardening into tiny, pearl-like cysts. They’re most noticeable around the delicate eye area, cheeks, and forehead because the skin there is thinner and turns over more slowly.
There are a few main types:
- Primary milia: These appear spontaneously and are common in both children and adults, often on the face or genitals.
- Secondary milia: These develop after skin trauma, such as burns, rashes, prolonged sun exposure, or heavy use of occlusive products like thick creams.
- Neonatal milia: Very common in newborns (affecting up to 40-50% of infants), usually resolving on their own without treatment.
Common triggers in adults include sun damage, long-term topical steroid use, or heavy, pore-trapping moisturizers—especially around the eyes. Dermatologists note that occlusive ingredients (like petroleum jelly in excess) can block natural exfoliation, trapping keratin and contributing to formation. They’re not contagious, not painful, and generally harmless, but their persistence can affect confidence.

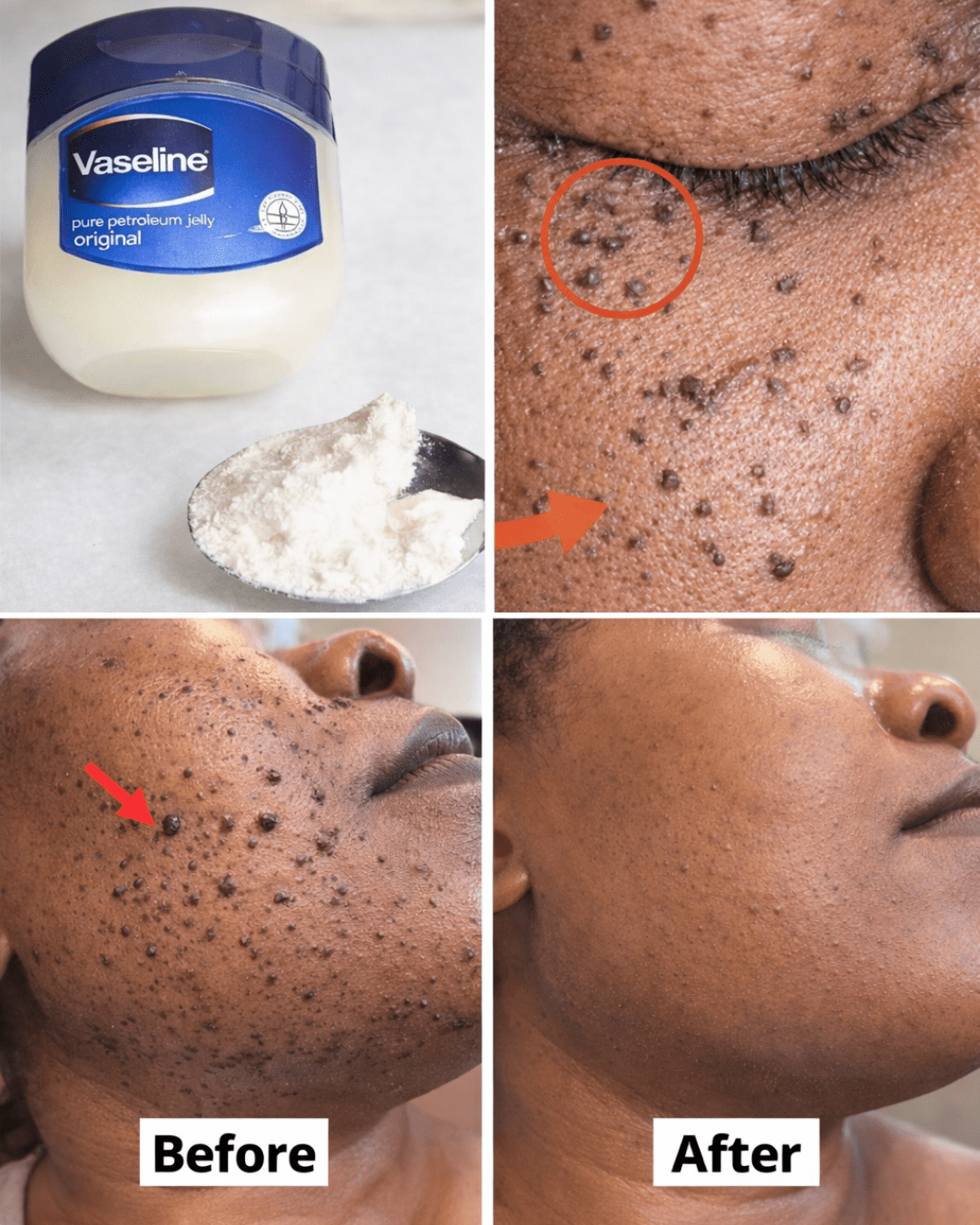
Why Viral “Overnight” Mixes Like Vaseline + Scrubs Often Backfire
Social media is full of quick-fix recipes—Vaseline mixed with sugar scrubs, baking soda pastes, or heavy occlusives promising fast removal. But dermatologists warn these can do the opposite.
Vaseline (petroleum jelly) is highly occlusive, meaning it seals the skin and prevents natural shedding. While great for very dry patches elsewhere, applying it thickly around the eyes can trap keratin and encourage more milia, according to expert insights. Abrasive scrubs (coffee grounds, baking soda) disrupt the skin’s pH and barrier, leading to dryness, redness, or irritation that might trigger secondary milia.
Evidence shows no strong studies support these DIY mixes for safe, effective removal—in fact, they often cause more problems than they solve. Gentle, consistent care outperforms risky shortcuts every time.

Safer Foundation: Gentle Exfoliation and Prevention Habits
The key to managing milia lies in promoting natural skin turnover without aggression. Here’s where evidence-based habits shine:
- Incorporate chemical exfoliants: Ingredients like salicylic acid (BHA) or glycolic acid (AHA) help dissolve dead cells and prevent buildup. Start with a gentle cleanser 2-3 times a week.
- Use retinoids wisely: Over-the-counter retinol or adapalene promotes cell turnover and can reduce milia over time. Begin slowly (a few nights per week) to avoid irritation.
- Choose lightweight moisturizers: Opt for non-comedogenic, gel-based formulas that hydrate without occluding pores.
- Apply broad-spectrum sunscreen daily: Sun damage is a major trigger for secondary milia—SPF 30+ protects and prevents worsening.
Always patch-test new products on a small area first. These steps, backed by dermatologist recommendations, support healthier skin texture without harsh interventions.
Momentum Builders: Daily Routines for Smoother Texture
Build a simple routine that encourages gradual improvement:
- Cleanse gently twice daily with a mild, non-stripping cleanser.
- Apply a warm compress for 5-10 minutes to soften the area (this can help loosen trapped material over time).
- Exfoliate chemically 2-3 times weekly with an AHA/BHA product.
- Moisturize lightly and follow with sunscreen in the morning.
- Avoid picking or squeezing at all costs—this prevents scarring and infection.
Consistency is crucial. Many see subtle improvements in weeks, with fuller results over months as skin turnover accelerates.
Advanced Care: When to See a Dermatologist
If milia persist despite gentle habits, professional help is safe and effective. Dermatologists perform manual extraction using a sterile lancet—quick, precise, and with minimal risk when done properly. Other options like minor procedures (e.g., cryotherapy or laser) may be suggested for clusters.
This approach is far superior to at-home attempts, reducing chances of complications while delivering clearer skin faster.
Ultimate Clarity: Prevention and Patience for Healthy Skin
Prevention boils down to supporting your skin’s natural processes: gentle exfoliation, sun protection, and avoiding heavy occlusives. Patience pays off—milia often improve with time and consistent care, and many resolve or fade significantly.
Here’s a quick comparison of approaches:
| Approach | Evidence Level | Safety | Effectiveness |
|---|---|---|---|
| Harsh DIY mixes | Low | Risky | Temporary / Irritating |
| Gentle skincare | Strong | High | Preventive / Gradual |
| Professional extraction | High | Excellent | Direct / Fast |
Achieve Smoother Skin: Your Gentle Milia Care Plan
Start today with one small change—swap your heavy eye cream for a lightweight, non-comedogenic option. Build from there: cleanse, exfoliate gently, protect with sunscreen. Over 30 days, this routine can lead to noticeably smoother texture and renewed confidence.
FAQ
How long do milia last in adults?
They can persist for months or longer without intervention, but gentle exfoliation and professional removal often speed resolution.
Can I prevent milia from coming back?
Yes—focus on daily sunscreen, lightweight products, and regular gentle exfoliation to support skin turnover and avoid triggers like heavy creams.
Are milia a sign of something serious?
No, they’re typically benign and cosmetic. However, if they appear suddenly in large numbers or with other symptoms, consult a dermatologist to rule out underlying issues.
This article is for informational purposes only and does not replace professional medical advice. Consult your healthcare provider or dermatologist for personalized guidance.