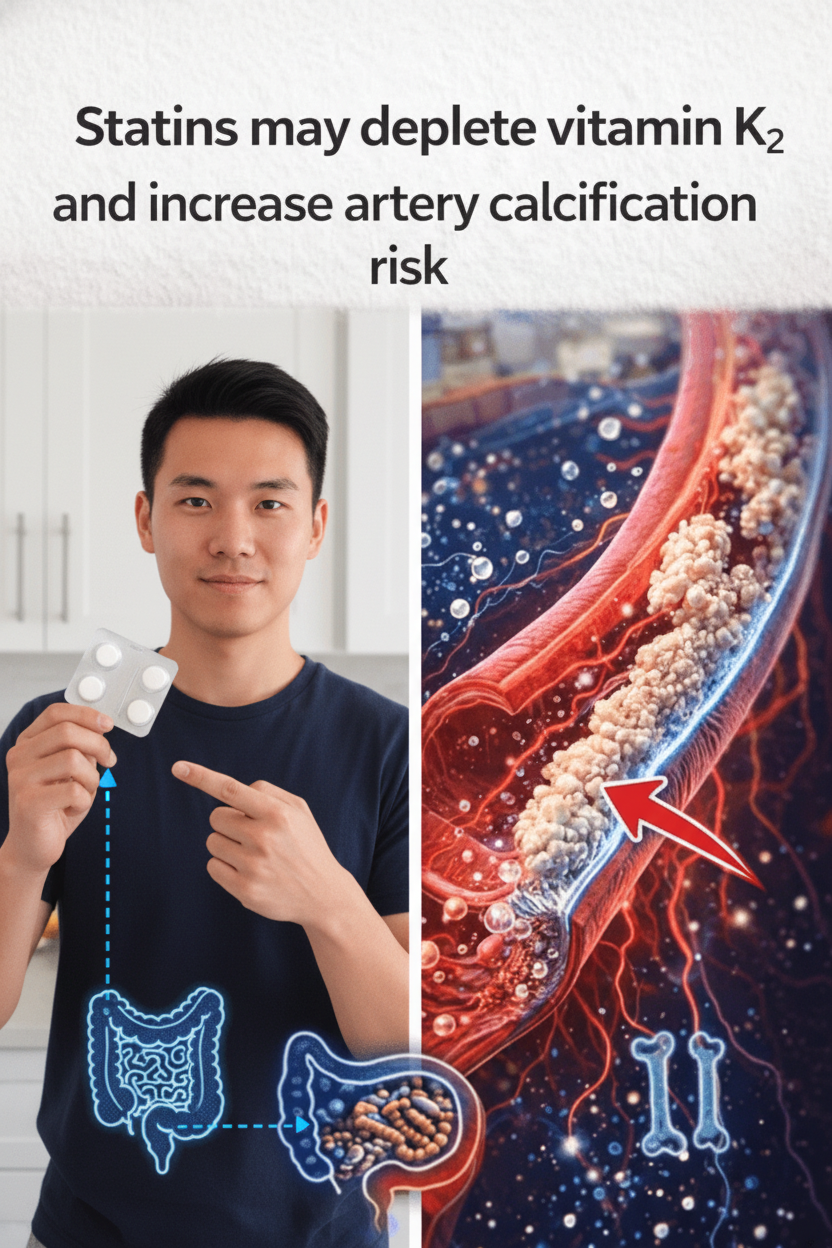
The Statin Paradox: Unraveling the Link Between Cholesterol Medication, Vitamin K₂, and Artery Health
For millions globally, statins represent a cornerstone of cholesterol management and a vital tool in safeguarding cardiovascular health. As some of the most widely prescribed medications, their efficacy in mitigating certain heart-related risks is well-established. However, a growing body of research is prompting an intriguing question about a subtle, potentially overlooked aspect: could statin therapy inadvertently impact the body’s vitamin K₂ activity, thereby influencing the long-term health and flexibility of your arteries? This presents a fascinating paradox – a medication designed to protect the heart might, through a complex biochemical pathway, affect processes crucial for maintaining pliable blood vessels. If you are among those relying on statins, understanding this potential interplay is undoubtedly important for your ongoing well-being. The encouraging news is that scientific inquiry is actively exploring nutritional approaches that could help address this emerging concern, and we will delve into the current evidence throughout this article.
Statins: Mechanism, Benefits, and an Emerging Question
Statins exert their primary effect by inhibiting HMG-CoA reductase, a crucial enzyme within the liver responsible for cholesterol synthesis. This targeted action effectively lowers circulating levels of LDL, often referred to as “bad” cholesterol, which in turn can significantly diminish the accumulation of atherosclerotic plaque within arterial walls for many individuals. Leading medical and public health organizations universally endorse statins as an indispensable intervention for bolstering cardiovascular health, particularly in populations presenting with elevated risk factors.
Nonetheless, like all pharmaceutical interventions, statin therapy warrants comprehensive consideration. While their prowess in reducing cholesterol is undeniable, a series of observational and mechanistic investigations have highlighted an intriguing association: some long-term statin users show an increase in coronary artery calcification (CAC). This refers to the deposition of calcium within the walls of the arteries, which can compromise their natural elasticity and function. This apparent contradiction—a medication designed to protect the heart potentially contributing to arterial stiffening—has presented a long-standing enigma for medical researchers.
The Crucial Role of Vitamin K₂ in Maintaining Arterial Flexibility
Vitamin K₂, scientifically known as menaquinone, is a vital fat-soluble nutrient sourced from specific dietary items such as fermented foods and certain animal products. Distinct from vitamin K₁—predominantly found in leafy green vegetables—K₂ performs critical functions beyond the liver. Its paramount role involves activating specialized proteins, notably Matrix Gla Protein (MGP). Activated MGP acts as a biological “calcium traffic controller,” effectively preventing calcium from depositing in soft tissues, such as arterial walls, and instead guiding it appropriately towards bone tissue for structural integrity. When the body maintains optimal vitamin K₂ levels, these proteins remain in their active state, thereby actively contributing to the resilience and health of arteries.
Extensive population-based research consistently demonstrates a strong correlation between suboptimal vitamin K status (often identified by elevated levels of inactive K-dependent proteins) and increased instances of arterial stiffness and calcification. This underscores vitamin K₂’s indispensable contribution to long-term vascular well-being.
The Potential Mechanism: How Statins May Influence Vitamin K₂ Metabolism
This is where the intricate connection between statins and arterial health truly deepens. Statins primarily target the HMG-CoA reductase enzyme, which is a key component of the mevalonate pathway—the very same biochemical route essential for cholesterol synthesis. Intriguingly, this mevalonate pathway is also implicated in critical metabolic processes, including the conversion of vitamin K₁ into its active forms of vitamin K₂ (specifically menaquinone-4, or MK-4) within various extra-hepatic tissues.
A growing body of scientific literature supports this potential interaction. For instance, a notable 2021 cross-sectional analysis published in the Kaohsiung Journal of Medical Sciences revealed that individuals taking statins exhibited significantly higher levels of inactive osteocalcin. This serves as a clinical biomarker indicative of reduced vitamin K activity within the body, particularly when compared to a control group of non-statin users. Furthermore, the study observed that statin users also presented with elevated coronary artery calcification scores, even after meticulous adjustment for other confounding variables. Numerous other reviews and mechanistic studies have posited that this interference with vitamin K metabolism could indeed be a contributing factor to the increased arterial calcification frequently observed in some individuals undergoing long-term statin therapy. Research consistently highlights links between statin use and alterations in the functionality of vitamin K-dependent proteins responsible for the precise regulation of calcium distribution throughout the body.
It is crucial to reiterate that this potential interaction does not negate the profound, well-documented benefits of statins for many patients. Not all calcification changes directly translate into adverse clinical outcomes. The paramount objective is to foster a comprehensive understanding of these complex metabolic pathways, empowering you to engage in informed discussions and collaborative decision-making with your healthcare provider regarding your treatment plan and overall wellness strategy.
Key Research Findings on the Statin-Vitamin K₂ Relationship
- Consistent Observational Data: A significant number of studies consistently report that individuals on statin therapy tend to exhibit elevated Coronary Artery Calcification (CAC) scores. A subset of this research further proposes a direct correlation between these higher calcification levels and compromised vitamin K status.
- Elucidated Mechanistic Pathways: Scientific investigations have provided robust mechanistic insights, indicating that by interfering with the mevalonate pathway, statins may inadvertently impair the body’s endogenous capacity to synthesize specific active forms of vitamin K₂. This impairment, in turn, can directly affect the proper activation of crucial proteins like Matrix Gla Protein (MGP), which are vital for calcium regulation.
- Nuanced Clinical Trial Outcomes: Clinical research presents a more complex picture. While some trials have not conclusively demonstrated a direct reversal of established arterial calcification through vitamin K₂ supplementation alone, other studies—particularly subgroup analyses involving statin users—offer promising suggestions regarding the potential for slowing the progression of calcification, especially when vitamin K₂ is administered in conjunction with vitamin D. It is paramount to emphasize that no extensive, conclusive studies currently assert that vitamin K₂ can reverse existing heart conditions or serve as a substitute for prescribed medical treatments. The overarching scientific consensus remains focused on the strategic importance of maintaining optimal nutrient balance as part of a holistic health strategy.
Proactive Considerations for Individuals on Statin Therapy
If you are currently prescribed statins and this information has raised questions or concerns regarding your arterial health, it is highly advisable to engage in a detailed discussion with your healthcare provider. Here are some evidence-informed considerations to bring to your next appointment:
- Discuss Your Vitamin K Status: Inquire with your doctor about assessing your vitamin K status. While routine, simple blood tests can measure certain markers (such as inactive osteocalcin) that provide insights into your body’s vitamin K activity, a comprehensive discussion with your physician can determine if such testing is appropriate for your individual health profile.