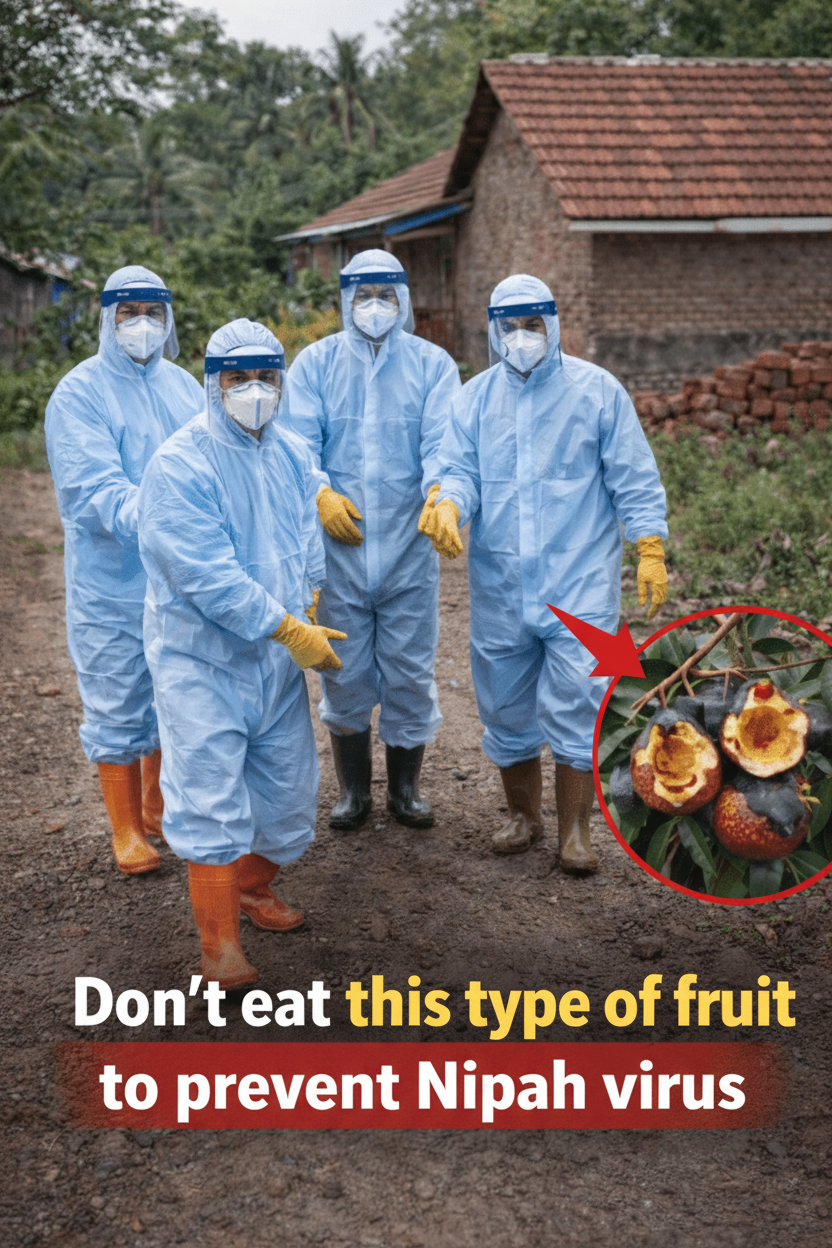
Nipah Virus Threat: The Critical Warning Against Consuming Bat or Bird-Contaminated Fruit
Across regions susceptible to Nipah virus outbreaks, leading health organizations such as the WHO, CDC, ICMR, and national health ministries in countries like India, Bangladesh, and Malaysia consistently issue a vital public health advisory. They strongly caution against consuming any fruit—particularly dates, mangoes, bananas, jackfruit, or any produce exhibiting bite marks or saliva residue—that has been partially eaten, gnawed, or otherwise contaminated by bats, birds, or other wildlife. This stringent recommendation is rooted in clear scientific understanding, which we will explore in detail.
Understanding Nipah Virus Transmission Through Contaminated Fruit
Fruit bats, specifically those of the Pteropus genus (commonly known as flying foxes), serve as the natural host for the Nipah virus. These bats carry the virus without displaying any symptoms themselves. However, they excrete the virus through their saliva, urine, and feces, particularly when they are foraging for food.
The transmission cycle often begins when bats feed on ripe fruits directly from trees. They typically take a few bites or lick the surface, leaving behind saliva that can contain significant viral loads. When humans (or intermediary animals like pigs) subsequently consume this contaminated fruit, the virus can be transmitted.
Historical outbreaks illustrate this pathway clearly. In Bangladesh, for instance, numerous infections have been traced back to individuals drinking raw date palm sap that was exposed to and contaminated by bat saliva or urine. Similarly, consuming fruits like mangoes, bananas, or jackfruit bearing visible bite marks or saliva residue has been definitively linked to Nipah virus transmission. Once ingested, the virus typically enters the human body via mucous membranes in the mouth and throat, or through small cuts, leading to severe illness.
Notable Nipah Outbreaks Linked to Contaminated Produce
- Malaysia (1998–1999): The initial significant Nipah outbreak saw the virus spill over from bats to pigs via contaminated fruit, subsequently spreading to humans.
- Bangladesh & India (Multiple outbreaks, 2001–2023): A majority of cases in these regions have been directly attributed to the consumption of raw date palm sap, which became contaminated by bats.
- Kerala, India (2018, 2021, 2023, 2024): Recurring outbreaks in Kerala have shown connections to direct contact with infected fruit bats or environments where contamination occurred.
Why This Nipah Prevention Advisory Is Paramount
The urgency behind this warning cannot be overstated, given the severe nature of Nipah virus infection. Here’s why vigilance is crucial:
- High Fatality Rate: Nipah virus boasts a chilling mortality rate, often ranging from 40% to 75% during outbreaks.
- No Specific Treatment or Vaccine: Currently, there is no approved vaccine to prevent Nipah, nor is there any specific antiviral medication to treat the infection. Patient care remains largely supportive.
- Risk of Human-to-Human Transmission: The virus can spread directly between people through close contact or respiratory droplets, meaning a single infected individual has the potential to initiate a wider chain of transmission.
- Virus Persistence: The Nipah virus can remain viable on fruit surfaces and within bat saliva for periods ranging from several hours to multiple days.
- Minimal Exposure, Maximum Risk: Even a seemingly insignificant bite mark or a tiny droplet of bat saliva on a piece of fruit can harbor sufficient viral particles to cause a human infection, particularly if the fruit is consumed raw or unwashed.
Essential Prevention Guidelines: Protecting Yourself from Nipah Virus
Public health officials recommend these straightforward yet critical steps to minimize your risk of Nipah virus exposure:
- Inspect Fruit Carefully: Absolutely avoid consuming any fruit that shows visible bite marks, chew marks, or traces of saliva. Similarly, do not eat fruit that has fallen from trees, as bats frequently drop partially consumed produce.
- Exercise Caution with Date Palm Sap: Refrain from drinking raw date palm sap (often known as toddy) unless you can confirm it has been collected and stored in a manner that completely protects it from bat contamination. Boiling the sap effectively inactivates the virus.
- Thoroughly Wash and Peel Produce: Always wash all fruits meticulously under running water, even if they appear unblemished. Peeling fruits when feasible adds an extra layer of safety.
- Steer Clear of Bat Roost Areas: Avoid collecting or eating any fruit found beneath trees known to house large bat colonies or roosts.
- Secure Food Storage: In regions where bats are prevalent, ensure all stored fruits and food items are adequately covered, using nets or screens to prevent any potential contamination.
The Crucial Takeaway on Nipah Virus Prevention
It’s important to clarify that this public health advisory is not a blanket recommendation to avoid all fruit. Instead, it’s a targeted warning against consuming fruit that has been compromised by bat saliva or urine. While Nipah virus infections are relatively rare, their appearance signifies an extremely dangerous health threat. The consumption of contaminated fruit stands out as one of the most direct and, crucially, preventable transmission pathways.
For individuals residing in or traveling to areas identified as high-risk for Nipah (such as Kerala in India, Bangladesh, and various parts of Southeast Asia), adhering to one straightforward principle can be life-saving: If a bat or bird has bitten it, do not eat it. A simple visual check can be the difference between safety and severe illness. This habit, once adopted, can protect lives, a lesson many families in affected outbreak zones have tragically learned too late.
Disclaimer
This article is provided strictly for informational purposes and should not be considered medical advice. Nipah virus infection represents a severe, potentially fatal illness. Should you experience symptoms such as fever, headache, vomiting, disorientation, seizures, or difficulty breathing following potential exposure to contaminated fruit/sap or contact with ill individuals/pigs in endemic regions, it is imperative to seek emergency medical care without delay. The prevention guidelines presented herein are derived from leading organizations including the WHO, CDC, and national health authorities in affected nations. Always prioritize and adhere to local health advisories issued during outbreaks.