Severe period cramps that leave you curled up in bed, pain during intimacy that strains relationships, chronic fatigue that makes daily life exhausting, and struggles with fertility that break your heart – if this sounds familiar, you’re not alone. Millions of women endure these debilitating symptoms for years, often dismissed as “normal” period pain or stress. But the reality is far more challenging: these could be signs of endometriosis, a chronic condition that disrupts lives in silence, with diagnosis often delayed by 7-9 years according to recent studies.
The frustration builds as symptoms worsen, impacting work, relationships, and mental health, leaving many feeling isolated and hopeless. Yet there’s hope – understanding this condition empowers you to seek proper care and manage it effectively. And later in this article, I’ll share practical steps that many women use to regain control… keep reading to discover what could change everything for you.

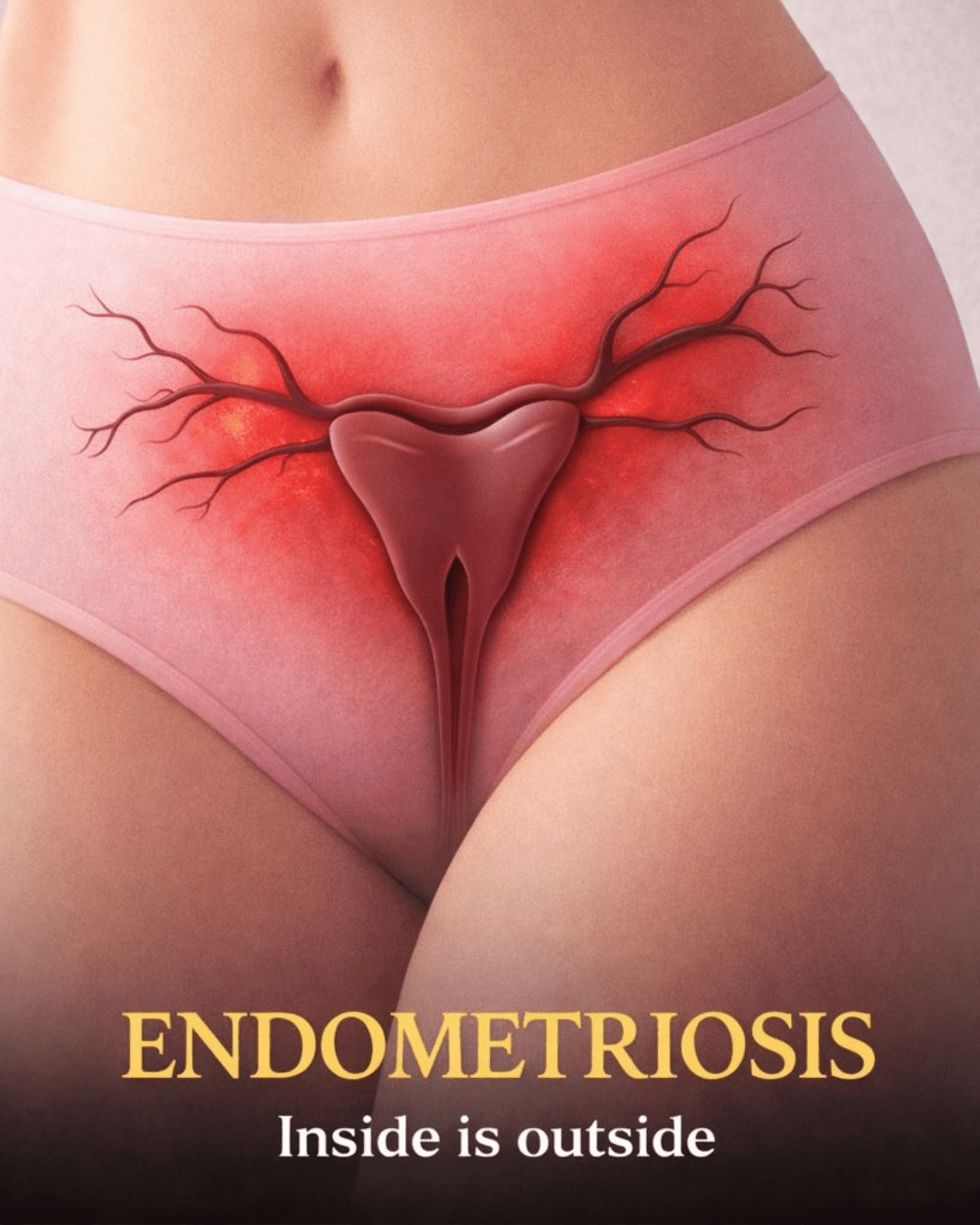
What Is Endometriosis?
Endometriosis occurs when tissue similar to the lining of the uterus (endometrium) grows outside the uterus. This misplaced tissue can appear on ovaries, fallopian tubes, the pelvic lining, or even beyond the pelvis.
Like normal endometrial tissue, it responds to hormonal changes:
- It thickens during the menstrual cycle
- It breaks down
- It attempts to shed
But here’s the catch – this tissue has no way to exit the body. Trapped blood causes inflammation, irritation, and eventually scar tissue or adhesions.
Research shows endometriosis affects about 10% of women of reproductive age worldwide – that’s over 190 million people. It’s a chronic, estrogen-dependent condition, but it’s not contagious or caused by anything you’ve done wrong.
But that doesn’t make it any less real or painful…

Common Symptoms of Endometriosis
Symptoms vary widely – some women experience mild discomfort, while others face debilitating pain. Pain is the hallmark, but it’s often unpredictable.
Here are the most common signs:
- Intense menstrual cramps that worsen over time or don’t improve with standard pain relievers
- Chronic pelvic pain, lower back pain, or abdominal discomfort unrelated to periods
- Pain during or after sexual intercourse (dyspareunia)
- Heavy periods, bleeding between cycles, or spotting
- Digestive problems like bloating, nausea, constipation, or diarrhea, especially during menstruation
- Fatigue and low energy that persists
- Difficulty conceiving (infertility affects 30-50% of women with endometriosis)
These overlap with conditions like IBS or PID, which is why many women suffer undiagnosed for years. The truth is, if your pain disrupts your life, it deserves attention – no matter what anyone says.

What Causes Endometriosis?
Scientists don’t know the exact cause yet, but several theories have strong support from research.
Possible contributing factors include:
- Retrograde menstruation: Menstrual blood flows backward through the fallopian tubes into the pelvis, implanting endometrial cells
- Genetic predisposition: If your mother or sister has it, your risk increases significantly
- Immune system issues: The body may not recognize and destroy misplaced tissue
- Hormonal influences: Estrogen promotes growth of endometrial-like tissue
Studies also link it to environmental factors and inflammation, but it’s not due to lifestyle alone. Importantly, endometriosis is not preventable through diet or exercise changes – though these can help manage symptoms.
This is the part where many women feel relieved: it’s not your fault.
How Is Endometriosis Diagnosed?
Diagnosis can be frustrating because there’s no simple blood test. Symptoms mimic other issues, leading to that average 7-9 year delay.
Doctors typically start with:
- A detailed history of your symptoms, periods, and family background
- Pelvic exam to check for abnormalities
- Imaging like ultrasound or MRI to spot cysts or deep lesions
The gold standard remains laparoscopy – a minimally invasive surgery to visualize and biopsy tissue. Advances in imaging are improving non-surgical detection, but confirmation often requires this procedure.
If you’re experiencing symptoms, don’t wait – track them and advocate for yourself.

Endometriosis and Fertility: What You Should Know
Endometriosis is a leading cause of infertility, affecting 30-50% of those trying to conceive.
How it impacts fertility:
- Scar tissue can block fallopian tubes
- Inflammation may affect egg quality or implantation
- Adhesions distort pelvic anatomy
The good news? Many women with endometriosis conceive naturally or with assistance like IVF. Early intervention improves outcomes, and surgery can help in mild cases.
If fertility is a concern, discuss it openly with a specialist – options exist.
Management and Treatment Options
There’s no cure yet, but effective ways to manage symptoms and improve quality of life exist. Treatment is personalized based on severity, age, and goals.
Common approaches include:
- Pain relief: Over-the-counter NSAIDs like ibuprofen for milder symptoms; prescription options for severe pain
- Hormonal therapies: Birth control pills, progestins, or GnRH agonists/antagonists to suppress menstruation and reduce growth
- Surgery: Laparoscopy to remove lesions, often providing significant relief; hysterectomy in severe, non-responsive cases
- Lifestyle support: Exercise, stress reduction, and complementary therapies like acupuncture
Research shows combining therapies often works best. Always consult a healthcare provider – what helps one person may differ for another.
Here’s a quick comparison:
| Treatment Type | Pros | Cons | Best For |
|---|---|---|---|
| Pain Medications | Quick relief, non-invasive | Doesn’t address root cause | Mild symptoms |
| Hormonal Therapy | Reduces pain and lesions | Side effects like mood changes | Ongoing management |
| Surgery | Can remove tissue, improve fertility | Invasive, possible recurrence | Severe cases or fertility goals |
The Role of Diet and Lifestyle in Managing Endometriosis
While diet doesn’t cause or cure endometriosis, emerging research suggests it can influence symptoms.
Studies indicate:
- Higher intake of red and processed meats may increase risk or worsen inflammation
- Anti-inflammatory foods (fruits, vegetables, omega-3s) may ease pain
- High-fiber diets could help balance hormones
- Reducing trans fats and focusing on plant-based options shows promise
An anti-inflammatory approach, like Mediterranean-style eating, supports overall health. But evidence is ongoing – no one diet fits all.
Practical Steps to Take Control Today
Ready for actionable tips? Here’s what you can do right now:
- Track your symptoms in a journal or app – note pain levels, triggers, and cycle patterns to share with your doctor
- Prioritize anti-inflammatory foods: Add more greens, berries, fatty fish, and nuts; limit red meat and processed foods
- Incorporate gentle movement: Walking, yoga, or swimming 30 minutes most days to reduce stress and pain
- Build a support network: Join online communities or local groups for shared experiences
- Schedule a specialist visit: Seek a gynecologist experienced in endometriosis if symptoms persist
Small changes add up – many women report better days with these habits.
Living Well With Endometriosis
This condition can affect every aspect of life, from career to relationships and emotional well-being. But with the right management, many thrive.
Connect with others, prioritize self-care, and remember: seeking help is strength, not weakness. Raising awareness reduces stigma and drives better care.
You’re not alone – and better days are possible. ❤️
Frequently Asked Questions
Is endometriosis curable?
No, there’s currently no cure, but symptoms can be effectively managed with treatment, and many women experience significant relief.
Can I get pregnant with endometriosis?
Yes – while it increases infertility risk, many conceive naturally or with help like fertility treatments. Early diagnosis helps.
Does endometriosis go away after menopause?
Symptoms often improve post-menopause due to lower estrogen, but some persist if scar tissue remains.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider with any questions about your health or a medical condition. Individual experiences with endometriosis vary, and treatments should be tailored by a doctor.