Imagine enduring crippling cramps every month that leave you curled up in bed, missing work, and feeling like no one truly understands. You’ve been told it’s “just bad periods” or that you should tough it out, but the pain keeps coming back—sometimes worse, sometimes joined by exhaustion, heavy bleeding, or even struggles to conceive. For millions of women, this isn’t just a bad period; it could be endometriosis, a chronic condition that often goes undiagnosed for years. The good news? Understanding it early can change everything—and there’s one key insight waiting at the end of this article that many women wish they’d known sooner.

What Is Endometriosis, and Why Does It Matter?
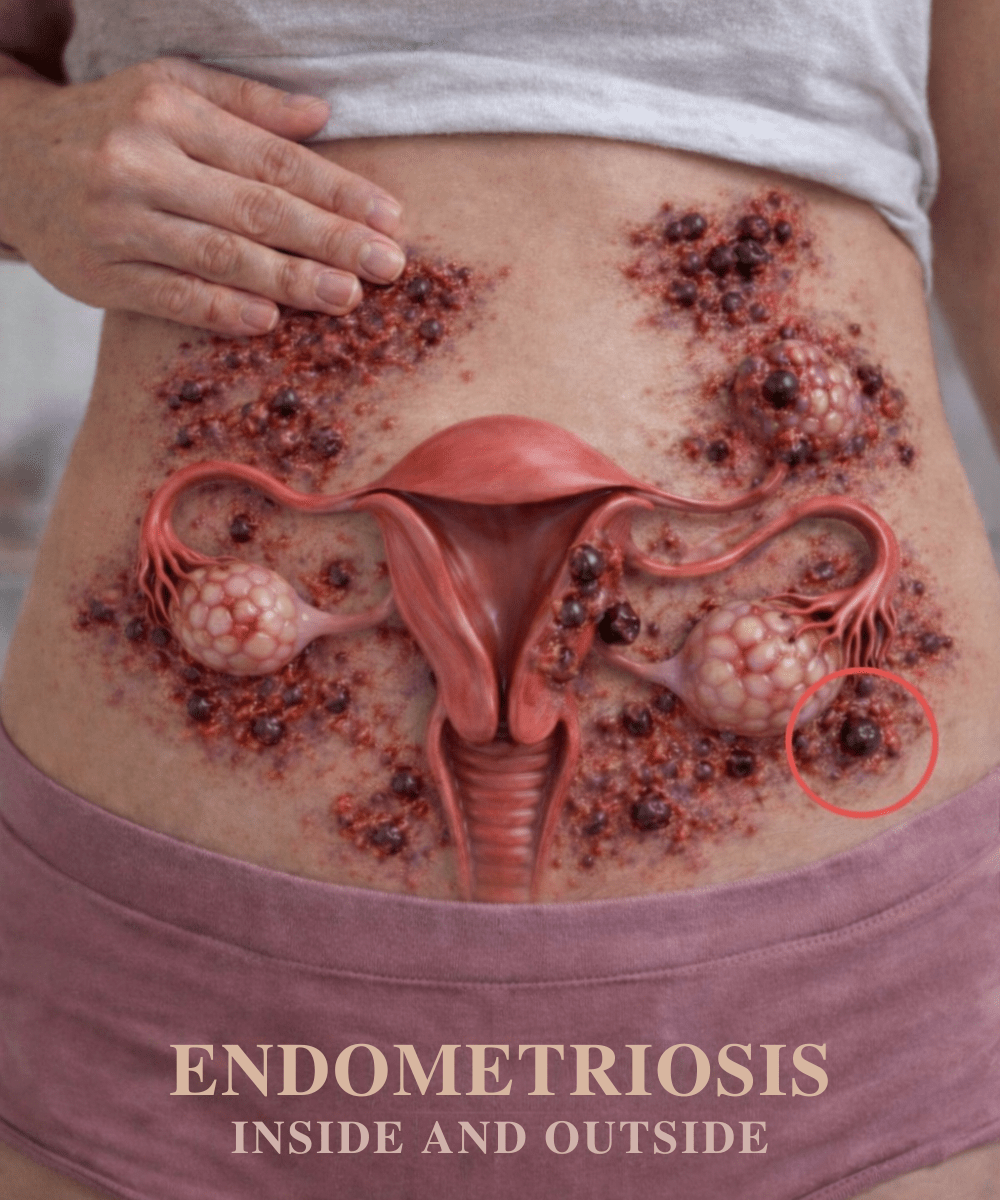
Endometriosis occurs when tissue similar to the lining inside the uterus (the endometrium) grows outside of it—on ovaries, fallopian tubes, pelvic lining, or even farther afield. Every month, this tissue responds to hormonal changes just like the uterine lining: it thickens, breaks down, and bleeds.
But unlike normal menstrual blood, this has nowhere to go. It becomes trapped, leading to inflammation, scar tissue, and adhesions (bands of fibrous tissue that can cause organs to stick together).
According to the World Health Organization, endometriosis affects roughly 1 in 10 women of reproductive age worldwide—that’s about 190 million people. Yet the average time from symptom onset to diagnosis is 7–10 years.
Why the delay? Symptoms are often dismissed as normal period discomfort or misattributed to stress, IBS, or other conditions.
The truth is, endometriosis can significantly impact daily life, relationships, work productivity, and mental health. But with awareness and proper management, many women lead fulfilling, active lives.

Common Symptoms of Endometriosis Every Woman Should Recognize
Symptoms vary widely—some women experience severe pain with minimal disease, while others have extensive growth but milder discomfort. Here are the most common signs:
- Severe menstrual cramps that don’t improve with over-the-counter pain relievers and may worsen over time

- Chronic pelvic pain that persists beyond periods, sometimes radiating to the lower back or legs

- Pain during or after intercourse (known as dyspareunia)
- Heavy or irregular menstrual bleeding, including spotting between periods
- Infertility or difficulty getting pregnant
- Digestive issues, especially bloating, diarrhea, constipation, or nausea that flare during menstruation

- Fatigue that feels overwhelming and unrelenting
- Painful bowel movements or urination, particularly during periods
These symptoms are often overlooked because they overlap with “normal” period experiences or other conditions. But if they interfere with your quality of life, they deserve attention.
What Causes Endometriosis? Current Theories and Risk Factors
Researchers still don’t know the exact cause of endometriosis, but several well-supported theories exist:
- Retrograde menstruation: Menstrual blood flows backward through the fallopian tubes into the pelvic cavity, allowing endometrial cells to implant and grow.
- Immune system dysfunction: The body may fail to recognize and clear misplaced endometrial-like tissue.
- Genetic factors: Having a close relative (mother, sister) with endometriosis significantly raises risk.
- Cellular transformation: Other cells in the body may transform into endometrial-like cells due to hormonal or environmental triggers.
Certain factors increase likelihood:
- Starting periods at an early age
- Short menstrual cycles (less than 27 days)
- Never having given birth
- Low body weight or structural abnormalities in the reproductive tract
While these don’t guarantee endometriosis, they highlight why some women are more susceptible.
How Endometriosis Is Diagnosed
Getting a proper diagnosis is crucial, yet it’s often the biggest hurdle. Here’s the typical process:
- Medical history and pelvic exam: Your doctor will discuss symptoms and perform a physical exam to check for cysts or tenderness.
- Imaging tests: Ultrasound or MRI can detect larger endometriomas (cysts) but may miss smaller lesions.
- Laparoscopy: Considered the gold standard, this minimally invasive surgery allows direct visualization and biopsy of suspicious tissue.
Many women see multiple providers before receiving an accurate diagnosis. Persistence pays off—don’t hesitate to seek a second opinion from a gynecologist experienced in endometriosis.
Management Options: Finding Relief That Works for You
There’s currently no cure for endometriosis, but symptoms can often be managed effectively. Treatment is highly individualized.
Pain Management
- Over-the-counter NSAIDs (like ibuprofen) taken proactively around periods
- Hormonal therapies (birth control pills, progestin IUDs, or GnRH agonists) to suppress menstruation and reduce tissue growth
Surgical Options
- Laparoscopic excision to remove endometrial lesions and adhesions—often provides significant relief
- In severe cases, hysterectomy may be considered, though it doesn’t always eliminate symptoms
Fertility Support
- Assisted reproductive technologies (like IVF) for women struggling to conceive
Lifestyle Strategies Backed by Research
Studies suggest certain habits can reduce inflammation and improve symptoms:
- Regular moderate exercise (yoga, walking, swimming)
- An anti-inflammatory diet rich in fruits, vegetables, omega-3s, and whole grains while limiting red meat and processed foods
- Stress-reduction techniques (mindfulness, therapy, adequate sleep)
- Heat therapy and gentle pelvic floor physical therapy
Here’s a quick comparison of common approaches:
| Approach | Best For | Potential Benefits | Considerations |
|---|---|---|---|
| Hormonal therapy | Pain & bleeding control | Reduces periods, shrinks tissue | Side effects vary; not suitable for all |
| Laparoscopic surgery | Severe pain or fertility issues | Direct removal, long-term relief | Recovery time; recurrence possible |
| Lifestyle changes | Overall symptom reduction | Improves energy, mood, inflammation | Requires consistency |
Actionable Steps You Can Take Today
If you suspect endometriosis, here’s what to do next:
- Track your symptoms for 2–3 cycles (note pain level, timing, triggers).
- Schedule an appointment with a gynecologist and bring your symptom log.
- Ask specifically about endometriosis if your concerns have been dismissed before.
- Consider consulting a specialist (endometriosis excision surgeon or reproductive endocrinologist).
- Start small lifestyle tweaks—add anti-inflammatory foods and gentle movement.
Early intervention can make a meaningful difference.
Final Thoughts: You’re Not Alone
Endometriosis is more than “bad periods.” It’s a legitimate medical condition that deserves recognition and proper care. By understanding symptoms, causes, and management options, you can advocate for yourself and find relief that improves daily life.
And that key insight? Many women experience dramatic improvement once they find the right treatment team—don’t settle until you do.
Frequently Asked Questions
Is endometriosis curable?
No, there’s no definitive cure, but symptoms can often be managed very effectively with medication, surgery, or lifestyle changes.
How common is endometriosis?
It affects approximately 10% of women of reproductive age globally—about 190 million people—according to the World Health Organization.
Can you get pregnant with endometriosis?
Yes, many women with endometriosis conceive naturally or with assistance. However, it can impact fertility, so early evaluation is helpful if pregnancy is a goal.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider about your symptoms or concerns. Individual experiences and outcomes vary.