Endometriosis: A Woman’s Guide to Understanding, Managing Symptoms, and Enhancing Daily Life
If you’re one of the millions of women grappling with debilitating menstrual cramps that disrupt your routine, persistent fatigue that makes even simple activities daunting, or unexplained pelvic discomfort that lingers month after month, know that you are not alone. These challenges can significantly impact personal relationships, professional life, and overall well-being, often leading to feelings of isolation and profound frustration. The encouraging news is that gaining a deeper insight into endometriosis can empower you to discover practical strategies to support your body and significantly improve your quality of life. As we progress through this comprehensive guide, we’ll also explore some surprisingly effective everyday habits that many women find invaluable in navigating this chronic condition.
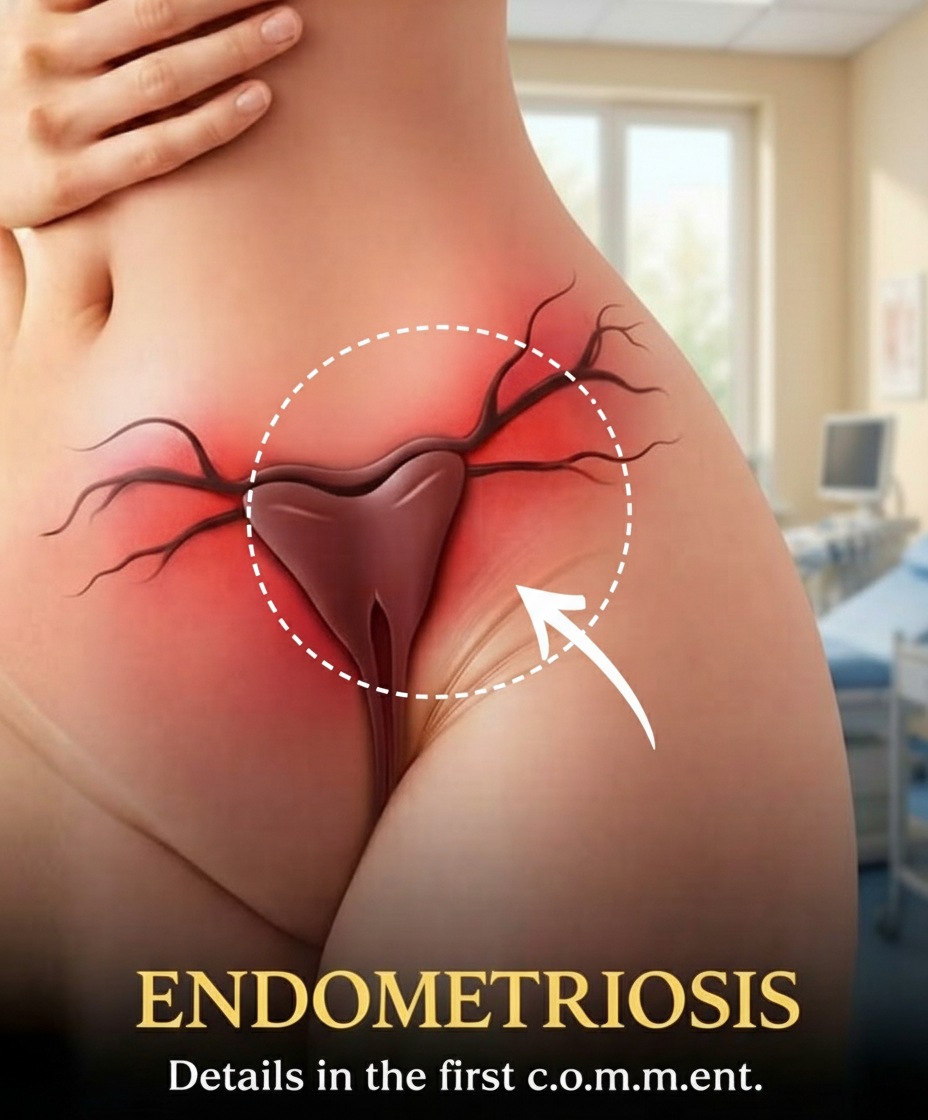
What Exactly Is Endometriosis?
Endometriosis is a prevalent chronic condition where tissue remarkably similar to the lining of the uterus (the endometrium) begins to grow outside the uterus. Most commonly, this misplaced tissue is found within the pelvic region, affecting organs like the ovaries, fallopian tubes, and the outer surface of the uterus. This ectopic tissue responds to the body’s hormonal fluctuations, particularly during the menstrual cycle, in the same way as the uterine lining. It thickens, breaks down, and attempts to shed blood. However, unlike menstrual blood that exits the body, this misplaced tissue has no escape route, leading to inflammation, irritation, and localized pain. Over time, this process can result in the formation of scar tissue and adhesions, which are fibrous bands that can bind organs together.
Research from esteemed organizations such as the World Health Organization indicates that endometriosis affects approximately 10% of women of reproductive age globally, translating to millions worldwide. Despite its widespread nature, many cases remain undiagnosed for years due to the varied and often overlapping nature of its symptoms, making early recognition a significant challenge.
Common Signs and Symptoms to Recognize
The presentation of endometriosis symptoms can differ dramatically from one individual to another, making it notoriously difficult to identify initially. However, several frequently reported signs warrant attention:
- Severe Menstrual Pain: Intense, often debilitating cramping during periods (dysmenorrhea) that tends to worsen over time, extending beyond typical period discomfort.
- Chronic Pelvic or Lower Back Pain: Persistent, deep-seated pain in the pelvic area or lower back that may not be exclusively tied to menstruation.
- Pain During or After Intercourse: Discomfort or pain experienced during or immediately following sexual activity (dyspareunia).
- Abnormal Bleeding: Menstrual periods that are unusually heavy (menorrhagia) or prolonged, as well as spotting or bleeding between cycles.
- Bowel and Bladder Issues: Difficulties with bowel movements (e.g., painful bowel movements, diarrhea, constipation) or urination, particularly flaring up around the menstrual period.
- Cyclical Digestive and Systemic Symptoms: Bloating, nausea, and profound fatigue that often occur in conjunction with the menstrual cycle.
Studies consistently reveal that these multifaceted symptoms often mimic those of other conditions, contributing to an average diagnostic delay of 7 to 10 years. The critical message here is that if pain is severely impacting your daily life and well-being, it is absolutely essential to seek a discussion with a healthcare provider. Early awareness and intervention can truly make a transformative difference.
Potential Factors Contributing to Endometriosis Development
While medical experts have yet to pinpoint a single, definitive cause for endometriosis, ongoing research has illuminated several theories and identified various risk factors. One prominent theory is retrograde menstruation, where menstrual blood containing endometrial cells flows backward through the fallopian tubes and into the pelvic cavity instead of exiting the body. Genetic predisposition also plays a significant role; if a close family member has endometriosis, your own likelihood of developing the condition may be elevated. Variations in the immune system are also being investigated, as an impaired immune response might prevent the body from effectively clearing misplaced endometrial-like tissue. Furthermore, hormones, particularly estrogen, are understood to influence the growth and persistence of this tissue.
It’s important to clarify that endometriosis is not solely caused by lifestyle choices, nor is it contagious or preventable through straightforward measures. The key takeaway here is that understanding these potential contributing factors helps to shift the focus towards effective supportive and management strategies rather than seeking a singular cure.
How Healthcare Providers Diagnose Endometriosis
Identifying endometriosis typically begins with a thorough and empathetic conversation about your medical history, lifestyle, and detailed symptom description. A physical examination, including a pelvic exam, can offer initial clues regarding tenderness or abnormalities. Imaging techniques, such as ultrasound or Magnetic Resonance Imaging (MRI), are often employed to visualize potential issues like endometriomas (cysts on the ovaries) or deep infiltrating endometriosis. However, for the most accurate and definitive diagnosis, a minimally invasive surgical procedure called laparoscopy is often performed. This involves a small incision through which a surgeon can directly visualize and, if necessary, biopsy any suspected endometrial implants.
Contemporary research consistently emphasizes that combining a comprehensive clinical evaluation with advanced imaging and, when appropriate, surgical confirmation leads to the best diagnostic outcomes. Encouragingly, increased public and professional awareness is now helping to shorten the diagnostic journey for many women worldwide.
Endometriosis and Its Impact on Fertility
Endometriosis is indeed linked to fertility challenges for a notable percentage of women. Studies suggest that between 30% and 50% of individuals with the condition may experience difficulties conceiving. The presence of inflammation, scar tissue, and adhesions can interfere with various stages of reproduction, including the release of eggs from the ovaries, the proper functioning of the fallopian tubes, and the successful implantation of an embryo in the uterus. That being said, it is crucial to remember that many women with endometriosis successfully achieve pregnancy, either naturally or with the aid of fertility treatments. If family planning is a consideration for you, initiating early discussions with a fertility specialist can illuminate helpful options and pathways. Understanding this connection empowers you to take proactive and informed steps regarding your reproductive health.
Everyday Habits and Strategies to Support Symptom Management
While professional medical guidance and treatment are absolutely essential for managing endometriosis, certain lifestyle approaches can play a significant complementary role, helping women feel more empowered and in control of their condition:
- Engage in Regular Gentle Movement: Activities like walking, swimming, yoga, or Pilates can help ease muscular tension, improve circulation, boost mood by releasing endorphins, and may even contribute to reducing systemic inflammation. Research consistently highlights the positive impact of physical activity on overall well-being and pain management.
- Prioritize Rest and Quality Sleep: Chronic pain and fatigue are common with endometriosis. Ensuring adequate, restorative sleep is crucial for the body’s healing processes and energy levels. Establishing a consistent sleep schedule and creating a relaxing bedtime routine can make a noticeable difference.
- Implement Stress-Reduction Techniques: Stress can exacerbate pain perception and inflammatory responses. Incorporate practices such as mindfulness meditation, deep breathing exercises, gentle stretching, or spending time in nature to help calm the nervous system and manage stress effectively.
- Utilize Heat Therapy: Applying warmth to the pelvic area can provide significant relief from cramping and muscle tension. This can be achieved through heating pads, warm baths, or hot water bottles.
- Explore Dietary Modifications: While not a cure, many women find relief by adopting an anti-inflammatory diet. This typically involves reducing processed foods, red meat, excessive sugar, and caffeine, while increasing intake of fruits, vegetables, whole grains, and omega-3 fatty acids. Consulting a nutritionist can provide personalized guidance.
- Consider Complementary Therapies: Some women find benefit from therapies such as acupuncture, massage therapy, or osteopathy to help manage pain and improve overall comfort. Always discuss these options with your healthcare provider to ensure they are appropriate for your individual situation.
By integrating these supportive habits into your daily life alongside medical treatment, you can actively participate in managing your endometriosis symptoms and significantly enhance your overall quality of life.