Many women in their 30s or early 40s start noticing changes like skipped periods, sudden waves of heat, or persistent tiredness that feel out of place for their age. These shifts can disrupt work, relationships, and self-confidence, often dismissed as “just stress” or temporary, while the real cause—a hormonal transition happening too soon—goes overlooked. The worry deepens when you realize early estrogen decline can affect fertility, bone strength, and heart health in ways that build quietly over time. But recognizing these signals now can open the door to timely support and better long-term outcomes. Stay with me as we explore the 10 key signs—and the straightforward steps that can help you regain control.

Why Early Menopause Is More Common Than Many Realize
Menopause typically arrives around age 51, but for some women, it comes much sooner. Premature menopause, also called primary ovarian insufficiency (POI), occurs before age 40 and affects about 1% of women. Early menopause, between ages 40 and 45, impacts around 5%, according to sources like the Mayo Clinic and Cleveland Clinic.
Factors like genetics, autoimmune conditions, cancer treatments (such as chemotherapy or radiation), surgical removal of ovaries, or even smoking can trigger this earlier shift. In many cases, the exact cause remains unknown.
The challenge? Symptoms often mimic everyday stress, leading to delayed awareness. But early recognition matters—it can help manage symptoms and reduce risks like osteoporosis and cardiovascular issues.
Curious how this might show up in your life? Let’s dive into the signs.
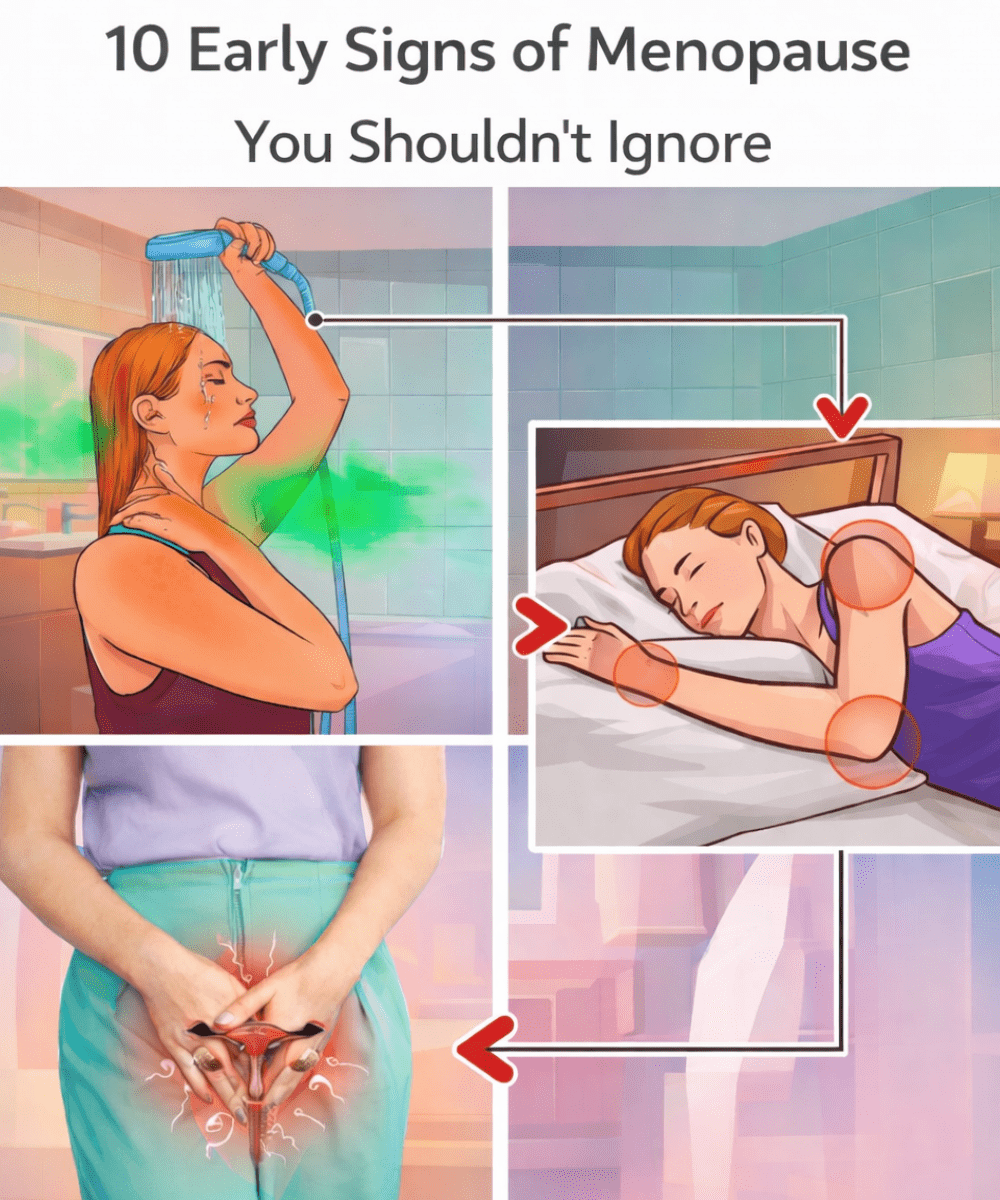
The 10 Critical Signs Your Body May Be Sending
These symptoms stem from declining estrogen levels. Not everyone experiences all of them, and they can vary in intensity. Tracking patterns helps spot trends.
1. Irregular or Missed Periods
This is often the first noticeable change. Cycles may become shorter, longer, heavier, or lighter—or skip months entirely.
Many women, like one patient who shared her story anonymously, noticed periods vanishing unpredictably in her late 30s, initially blaming work pressure. Research confirms irregular cycles as a hallmark sign.
Quick tip: Start logging your cycles today using an app or calendar. Patterns provide valuable clues.

2. Hot Flashes and Night Sweats
Sudden warmth spreading across your chest, face, and body—sometimes with sweating or chills—can strike day or night.
Up to 75% of women in menopause experience these vasomotor symptoms, often more intensely in early cases, per Cleveland Clinic data.
Imagine waking soaked in the middle of the night, exhausted before the day begins. Layered clothing and cooler bedding can offer immediate relief.
3. Sleep Disturbances
Night sweats or hormonal shifts can interrupt deep rest, leaving you tired despite a full night’s “sleep.”
Poor sleep compounds fatigue and mood challenges. Consistent bedtime routines help many women.

4. Mood Swings or Increased Anxiety
Feeling more irritable, tearful, or anxious than usual? Estrogen influences brain chemistry, including serotonin pathways.
Studies note higher risks of mood changes during hormonal transitions. Gentle movement or talking to a trusted friend can ease the edge.
5. Vaginal Dryness and Discomfort
Declining estrogen thins vaginal tissues, leading to dryness, itching, or pain during intimacy.
This common issue affects comfort and relationships but responds well to moisturizers or lubricants.
6. Persistent Fatigue
Unexplained tiredness that rest doesn’t fix can feel overwhelming.
Hormonal fluctuations sap energy levels. Small, balanced meals and hydration often make a difference.
7. Brain Fog and Memory Lapses
Trouble concentrating or recalling words mid-sentence?
Cognitive shifts are recognized in menopause research. Short breaks and focus exercises support clarity.

8. Joint or Muscle Aches
New stiffness or discomfort, sometimes mistaken for overexertion.
Lower estrogen can contribute to inflammation. Regular movement keeps joints flexible.
9. Urinary Changes
More frequent urges or occasional leaks when coughing or laughing.
Tissue changes affect bladder support. Pelvic floor exercises strengthen control.
10. Fertility Challenges
Difficulty conceiving despite trying?
Ovarian reserve naturally declines earlier in these cases. Early consultation opens options like preservation.
But here’s the encouraging part: many women manage these effectively with the right guidance.
Why These Signs Deserve Attention
Beyond daily discomfort, early estrogen loss accelerates risks for bone density reduction, heart health changes, and cognitive shifts—issues research links to longer-term well-being.
The upside? Proactive steps, discussed with a healthcare provider, can significantly support bone, heart, and overall vitality.
Next Steps: What You Can Do Right Now
If several signs resonate, start here:
- Track symptoms for 1-2 months—note frequency and triggers.
- Schedule a provider visit — especially if under 45 with irregular periods or other changes.
- Request tests like FSH (follicle-stimulating hormone) and estradiol levels to assess ovarian function.
- Discuss options — Hormone replacement therapy (HRT) until typical menopause age may be considered for symptom relief and risk reduction, weighing benefits and personal factors.
- Adopt supportive habits:
| Habit | Potential Benefit |
|---|---|
| Weight-bearing exercise (walking, strength training) | Supports bone density |
| Calcium-rich foods + vitamin D | Builds stronger bones |
| Balanced diet with phytoestrogens (soy, flax) | May ease mild symptoms |
| Stress reduction (yoga, meditation) | Improves sleep and mood |
| Quit smoking | Slows further estrogen decline |
These foundational changes complement medical guidance.
Imagine Feeling More in Control
Picture waking refreshed, managing flashes with ease, and knowing you’re protecting your future health. Many women report renewed energy and confidence after addressing this early.
You’re already ahead by reading this far—take that next small step today.
Frequently Asked Questions
What exactly is early menopause?
Early menopause occurs between ages 40-45, while premature (POI) is before 40. Both involve ovaries producing less estrogen sooner than average.
What causes it?
Common triggers include genetics, autoimmune disorders, medical treatments like chemotherapy, surgery, or unknown factors. Smoking can advance timing.
When should I see a doctor?
If you’re under 45 and experiencing irregular periods, hot flashes, or multiple symptoms above—especially if concerned about fertility—consult promptly for evaluation.
This article is for informational purposes only and does not replace professional medical advice. Always consult your healthcare provider for personalized guidance based on your health history.
(Word count: approximately 1,250)