Decoding Your Uterus: 12 Critical Warning Signs for Optimal Women’s Health
As women approach and pass the age of 40, it’s common to experience shifts in their menstrual patterns, pelvic sensations, or general vitality. These evolving symptoms are often mistakenly attributed to the natural aging process and brushed aside. However, these changes can be both frustrating and disruptive, frequently impacting daily routines, professional life, and personal relationships.
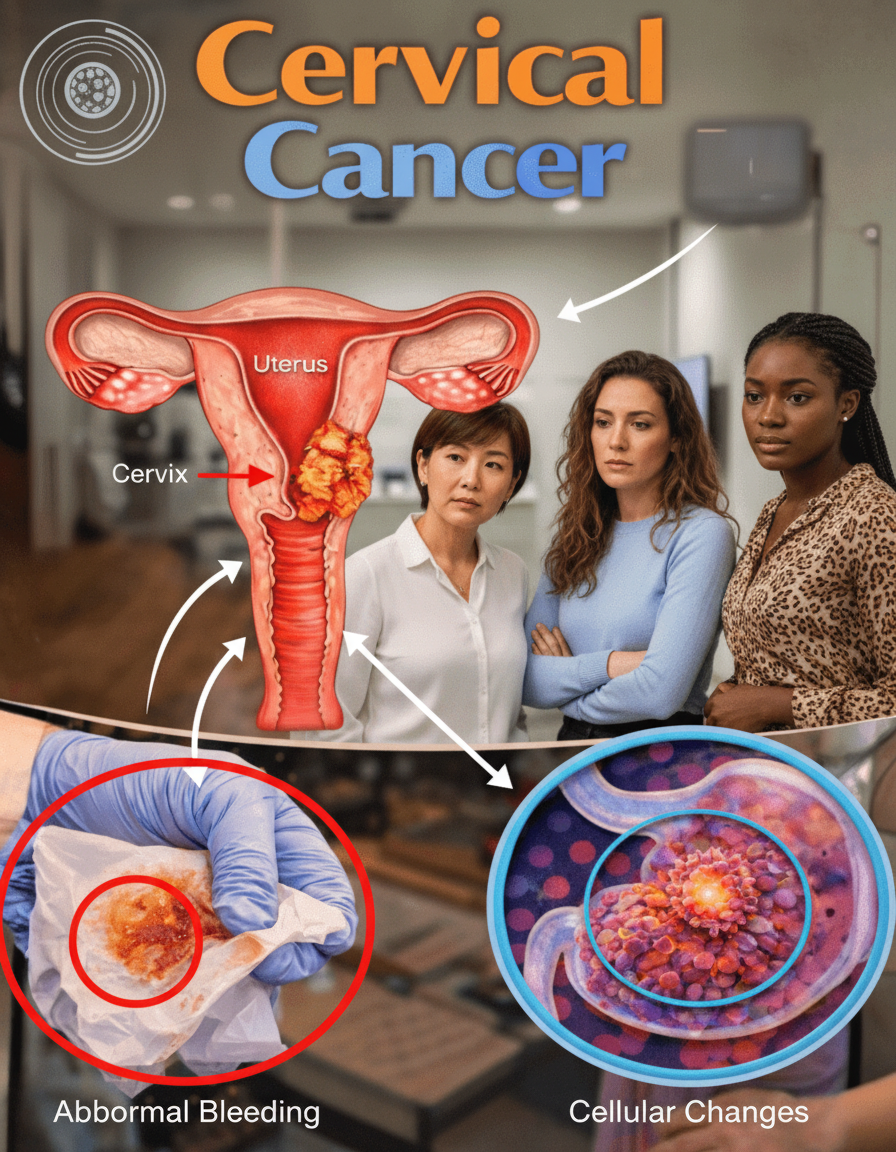
What may begin as intermittent discomfort could, in fact, signal deeper uterine health issues such as uterine fibroids, endometriosis, adenomyosis, or significant hormonal shifts associated with perimenopause. Early recognition of these emerging patterns holds the potential to profoundly improve your overall well-being and quality of life.
The encouraging news is that proactively listening to your body and openly discussing any changes with a healthcare professional can significantly enhance management and outcomes. This comprehensive guide delves into 12 prevalent warning signs that warrant your careful attention, supported by the latest medical research and expert insights. Stay with us to discover actionable steps you can implement immediately, along with an often-overlooked connection many women might not consider.
The Unspoken Challenges of Uterine Health
As women transition into their 40s and beyond, hormonal fluctuations become increasingly pronounced. Medical studies indicate that uterine fibroids affect a substantial 70-80% of women by age 50, with even higher prevalence in specific demographics. Similarly, conditions like endometriosis and adenomyosis often become most symptomatic around this life stage.
These gynecological issues can manifest in a range of symptoms that significantly diminish one’s quality of life, from heavy and prolonged bleeding to persistent, debilitating fatigue. Many women unfortunately delay seeking medical advice, assuming these are merely ‘part of getting older.’ However, promptly addressing these critical signals can prevent their escalation and lead to more effective management. Let’s explore these key uterine warning signs one by one.
Sign #1: Irregular Menstrual Cycles
If your menstrual periods are becoming unpredictable – whether you’re skipping months, experiencing cycles that are too frequent, or noticing wild variations in their duration – these irregularities could indicate underlying hormonal shifts or more specific uterine concerns. Research published in women’s health journals consistently links irregular periods to the onset of perimenopause or conditions like uterine fibroids. Diligently tracking your cycle using a simple app or calendar can help you identify patterns and provide valuable information for your doctor. Many women find considerable relief simply in understanding the potential causes behind their changing cycles.
Sign #2: Abnormally Heavy Periods (Menorrhagia)
Experiencing a need to change sanitary pads or tampons every hour or two, or having menstrual bleeding that extends beyond seven days, is a common and concerning complaint. Excessively heavy menstrual flow is a hallmark symptom of uterine fibroids and adenomyosis, as highlighted by reputable sources such as the Cleveland Clinic and reviews in Obstetrics & Gynecology. Such significant blood loss can lead to chronic tiredness and even anemia. If this description resonates with your experience, documenting the volume and duration of bleeding over a few cycles will be immensely helpful when consulting your physician.
Sign #3: Debilitating Menstrual Cramps (Dysmenorrhea)
Menstrual cramps that are so severe they disrupt your daily activities – forcing you to miss work or requiring strong pain medication – go far beyond typical discomfort. Numerous gynecologic studies connect severe dysmenorrhea to conditions such as endometriosis and adenomyosis. While heat packs, gentle movement, or relaxation techniques may offer temporary relief for some, persistent and incapacitating pain unequivocally warrants professional medical evaluation.
Sign #4: Persistent Pelvic Discomfort Beyond Your Period
An aching sensation or pressure in the lower abdomen that isn’t directly tied to your menstrual cycle can be a source of significant concern. This type of non-cyclical pelvic pain is frequently associated with fibroids, ovarian cysts, or other sources of uterine pressure, as documented in gynecology research. It’s particularly important to pay attention if this discomfort intensifies with physical activity or prolonged periods of sitting.
Sign #5: Unexplained Abdominal Bloating or Fullness
Feeling chronically swollen or experiencing a sensation of being “pregnant-looking” even when you are not menstruating is a common symptom linked to larger fibroids or adenomyosis. This persistent pressure or fullness in the abdomen can last for days or even weeks. While temporary relief might be found through dietary adjustments like reducing salt intake and maintaining adequate hydration, the underlying cause needs investigation.
Sign #6: Painful Intercourse (Dyspareunia)
Discomfort or pain experienced during or after sexual intimacy, medically known as dyspareunia, can place a significant strain on relationships and negatively impact self-confidence. Endometriosis is a frequent cause of this symptom, according to sources in sexual medicine and gynecology. Open communication with your partner and exploring different positions or lubrication can provide some temporary ease while you seek a comprehensive medical evaluation.
Sign #7: Chronic, Unexplained Fatigue
Experiencing constant tiredness, even after adequate rest, is often a subtle yet critical warning sign. This persistent fatigue can be directly connected to heavy menstrual bleeding leading to anemia, or to broader hormonal disruptions. Endocrinology studies frequently link ongoing fatigue to these systemic imbalances. Prioritizing sufficient sleep, focusing on nutrient-rich nutrition, and incorporating light exercise can support overall energy levels, but the root cause of the fatigue should be identified.
Sign #8: Increased Urinary Frequency or Urgency
Needing to use the bathroom more often than usual, especially during the night, or experiencing a sensation of incomplete bladder emptying, can result from uterine fibroids pressing directly on the bladder. Urology reports consistently confirm this pattern. While staying well-hydrated and avoiding bladder irritants like caffeine can temporarily alleviate symptoms, it’s crucial to understand if uterine pressure is the underlying factor.
Proactive Steps for Uterine Wellness
While monitoring symptoms is vital, incorporating certain lifestyle adjustments can also support your uterine health and overall well-being. Here are some quick, actionable steps many women find beneficial:
- Track Your Cycles and Symptoms: Maintain a daily journal or use a dedicated app to meticulously record your menstrual cycles, the nature of your bleeding, and any accompanying symptoms. This detailed information is invaluable for your healthcare provider.
- Embrace Anti-Inflammatory Nutrition: Incorporate a diet rich in anti-inflammatory foods. This includes an abundance of fruits, vegetables, whole grains, and healthy fats like omega-3 fatty acids found in fish and flaxseeds.
- Prioritize Regular Movement: Engage in moderate physical activity consistently. Exercise can help manage weight, improve circulation, and potentially alleviate some symptoms associated with uterine conditions.
- Manage Stress Effectively: Chronic stress can impact hormonal balance. Explore stress-reduction techniques such as mindfulness, yoga, meditation, or spending time in nature.
- Ensure Adequate Sleep: Quality sleep is foundational for hormonal regulation and overall health. Aim for 7-9 hours of uninterrupted sleep each night.
Remember, your body communicates with you through these signs. Paying attention and seeking professional medical advice when changes occur is the most empowering step you can take towards maintaining optimal uterine health and overall vitality. Don’t dismiss these messages; your well-being depends on it.
”
}
“`