Decoding Your Digestive Health: What Your Stool’s Color and Shape Tell You
Many of us diligently track our diet, fitness routines, and sleep patterns as pillars of good health. Yet, a crucial daily indicator often goes overlooked: what happens in the bathroom. The characteristics of your stool—its color, texture, and form—offer surprisingly profound insights into the efficiency of your digestive system, from nutrient absorption to hydration levels. Neglecting these daily signals might mean missing early warnings of internal imbalances.
However, by learning to recognize what constitutes a healthy bowel movement versus changes that warrant attention, you can gain a much clearer understanding of your body’s inner workings. And, as we’ll explore towards the end of this guide, adopting one simple habit could significantly improve your digestive regularity and overall well-being.
What Constitutes a Healthy Stool?
Ideally, healthy stool typically presents as a medium to dark brown shade. This coloration is a result of bile, produced by your liver, mixing with waste as it navigates through your intestinal tract. Medical experts, including those at institutions like the Cleveland Clinic and Mayo Clinic, explain that this distinctive brown hue primarily comes from bilirubin, a byproduct generated during the breakdown of old red blood cells.
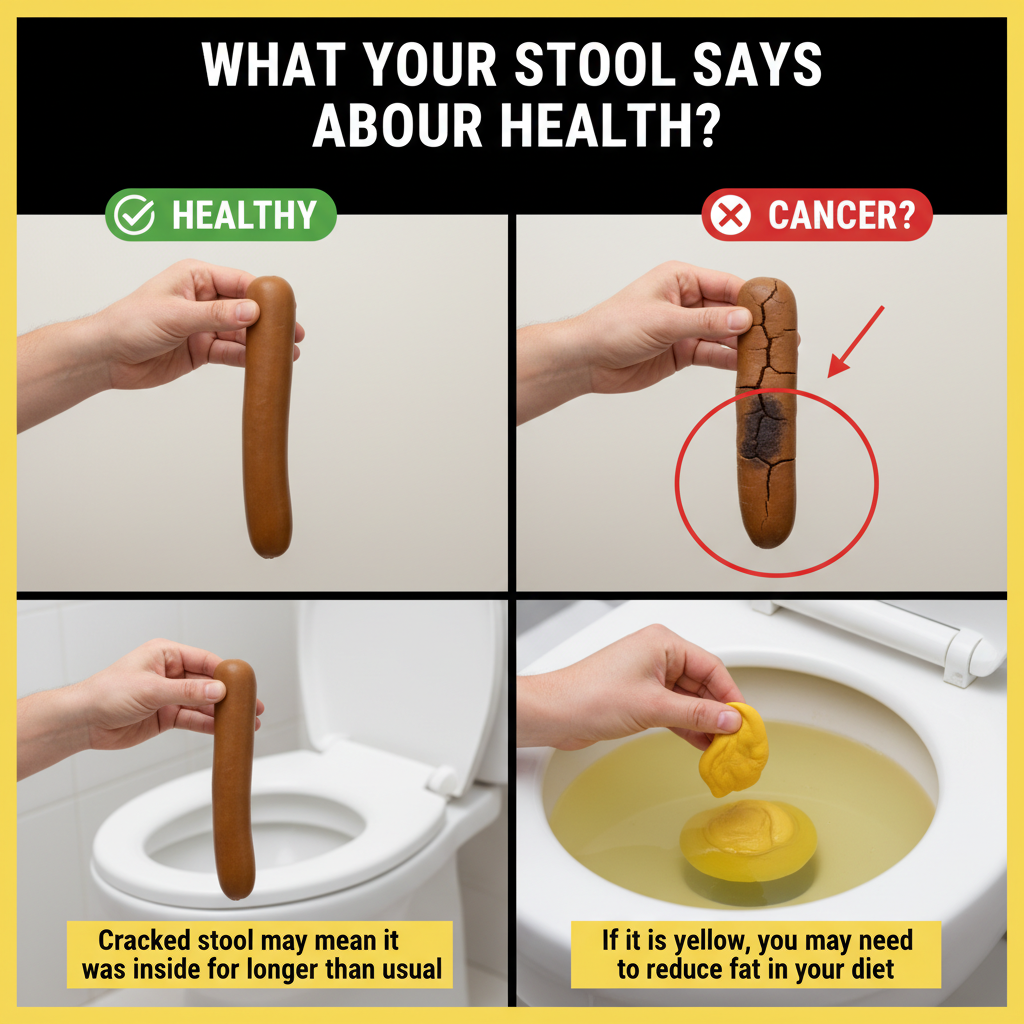
When it comes to shape and consistency, the Bristol Stool Chart—a widely accepted diagnostic tool developed by doctors at Bristol Royal Infirmary—classifies the most desirable stool types as:
- Type 3: Resembling a sausage with minor cracks on its surface – indicating a healthy consistency that’s easy to pass.
- Type 4: Smooth, soft, and snake-like – often regarded as the “gold standard” for comfortable and efficient bowel movements.
These ideal types suggest adequate dietary fiber intake, proper hydration, and a balanced transit time through your digestive system. If your bowel movements consistently align with these descriptions, your digestive health is likely in excellent shape. But what if they don’t? Let’s delve deeper into common variations and their potential meanings.
Common Stool Shapes and What They Might Indicate
The Bristol Stool Chart provides a comprehensive classification of seven different stool types, serving as an invaluable tool for tracking changes in your bowel patterns over time:
- Types 1-2 (Hard, Lumpy, or Pellet-Like): Stool that appears as separate hard lumps or a lumpy sausage often signals constipation. This occurs when stool remains in the colon for too long, allowing excessive water absorption. Research frequently links these types to insufficient fiber in the diet and a lack of physical activity.
- Types 5-7 (Soft Blobs to Fully Watery): On the other end of the spectrum, very soft, mushy, or entirely liquid stools suggest a rapid transit time through the intestines. These can be indicative of loose stools or diarrhea, which may result from dietary changes, heightened stress levels, or gastrointestinal infections.
Persistent occurrences of either extreme on the Bristol Stool Chart, especially when accompanied by discomfort, abdominal pain, or other unusual symptoms, warrant careful attention. However, the story doesn’t end with shape; color adds another critical layer of diagnostic information.
Revealing Insights from Stool Colors
While brown is the universally recognized norm, various other shades can appear due to dietary choices, medications, or specific digestive processes. Here’s a comprehensive breakdown, informed by reliable medical sources:
- Green Stool: Often benign, this can result from consuming large amounts of leafy green vegetables, certain food dyes, or if stool passes too quickly through the intestines, preventing bile from fully breaking down. It typically resolves without intervention.
- Yellow or Greasy Stool: This appearance, particularly if foul-smelling or floating, may point to issues with fat absorption. Potential underlying causes can include problems with the gallbladder, pancreas, or liver function. If persistent, monitoring and medical consultation are advisable.
- Black or Very Dark Stool: While sometimes caused by iron supplements, dark-colored foods like black licorice, or bismuth-containing medications (e.g., Pepto-Bismol), a tarry, sticky black stool could indicate bleeding in the upper digestive tract. Always seek professional medical evaluation if this occurs without a clear dietary or medicinal explanation.
- Red or Maroon Stool: Bright red blood often originates from lower intestinal sources, such as hemorrhoids or fissures. However, red stool can also be a harmless result of eating beets or red food dyes. Any persistent red stool without an obvious dietary cause requires prompt medical assessment.
- Pale, Clay-Colored, or Gray Stool: This concerning coloration may signal a reduction or blockage in bile flow, potentially indicating issues with the liver or bile ducts. Medical authorities like the Mayo Clinic strongly advise consulting a doctor for any ongoing pale or clay-colored stools.
Occasional, temporary shifts in stool color or consistency due to diet are common. Nevertheless, any lasting or unexplained changes should always prompt a closer examination and professional medical advice.
Everyday Habits to Foster Optimal Bowel Health
Achieving consistent, comfortable, and healthy bowel movements is often within reach through the implementation of simple, sustainable daily practices. Here’s how you can cultivate them:
- Gradually Increase Fiber Intake: Aim for 25-35 grams of dietary fiber daily, primarily from whole foods. Soluble fiber (found in oats, apples, and beans) helps to soften stool, while insoluble fiber (from whole grains, vegetables, and nuts) adds necessary bulk, facilitating easier passage.
- Prioritize Adequate Hydration: Drink at least 8-10 glasses of water daily. This intake should increase if you are boosting your fiber consumption, as water is crucial for keeping stool soft and ensuring smooth movement through the intestines.
- Engage in Regular Physical Activity: Even moderate exercise, such as 30 minutes of walking, yoga, or light cardio most days of the week, can significantly stimulate intestinal motility and promote regularity in bowel movements.
- Establish a Consistent Routine: Try to schedule your bowel movements around the same time each day. Respond promptly to the urge to go, and consider adopting a proper posture (e.g., using a footstool to elevate your feet slightly) to ease straining and facilitate a more complete evacuation.
These habits, widely supported by digestive health guidelines, are fundamental to promoting steady bowel patterns and preventing extremes like constipation or diarrhea.
When Changes Necessitate Professional Medical Input
While most minor fluctuations in stool appearance are temporary and harmless, certain persistent or severe symptoms warrant immediate medical attention. Consult a healthcare professional if you experience:
- Persistent changes in stool color, shape, or consistency lasting more than a few days.
- Severe abdominal pain or cramping accompanying bowel changes.
- Unexplained weight loss.
- Fever or chills alongside digestive symptoms.
- Any signs of blood in your stool (bright red, maroon, or tarry black) without a clear, benign explanation.
Early detection and professional guidance are key to addressing potential underlying health issues and maintaining optimal digestive wellness.