Our bodies possess an incredible ability to communicate, often sending subtle cues long before a serious health issue demands undeniable attention. Cervical cancer, a prevalent cancer impacting women globally, frequently develops without presenting clear initial symptoms. Consequently, many women inadvertently dismiss early indications, attributing them to typical hormonal fluctuations or minor infections. However, leading health organizations such as the Mayo Clinic and the American Cancer Society consistently highlight that early recognition of these often-understated warning signs can dramatically improve treatment outcomes. When detected promptly, cervical cancer is often highly treatable. What many women might scroll past, however, is that the most critical sign isn’t always the most dramatic; it’s often something persistent and easily overlooked. Continue reading to uncover eight essential symptoms and actionable steps to safeguard your well-being.
Why Cervical Cancer Deserves Your Attention
Cervical cancer originates in the cells of the cervix, which is the narrow, lower section of the uterus connecting to the vagina. This disease continues to be a significant global health challenge, with the World Health Organization reporting hundreds of thousands of new diagnoses annually, predominantly linked to persistent infections with high-risk human papillomavirus (HPV). The encouraging news is that this cancer is largely preventable and, when caught early, highly curable. Proactive measures like consistent screenings and heightened awareness are crucial for identifying cellular changes before they escalate. Given that early-stage cervical cancer often presents no discernible symptoms, routine Pap tests and HPV screenings are absolutely indispensable. As the disease progresses, more noticeable, yet still subtle, indications may emerge. While certain factors like being over 30, having a history of HPV exposure, smoking, or deferring recommended screenings can increase risk, it’s important to remember that no woman is entirely exempt. Overlooking unexplained bodily changes can permit the condition to advance, potentially leading to more complex health issues. Truly, your body is a constant communicator; developing the ability to interpret its signals is one of the most impactful actions you can take for your long-term health.
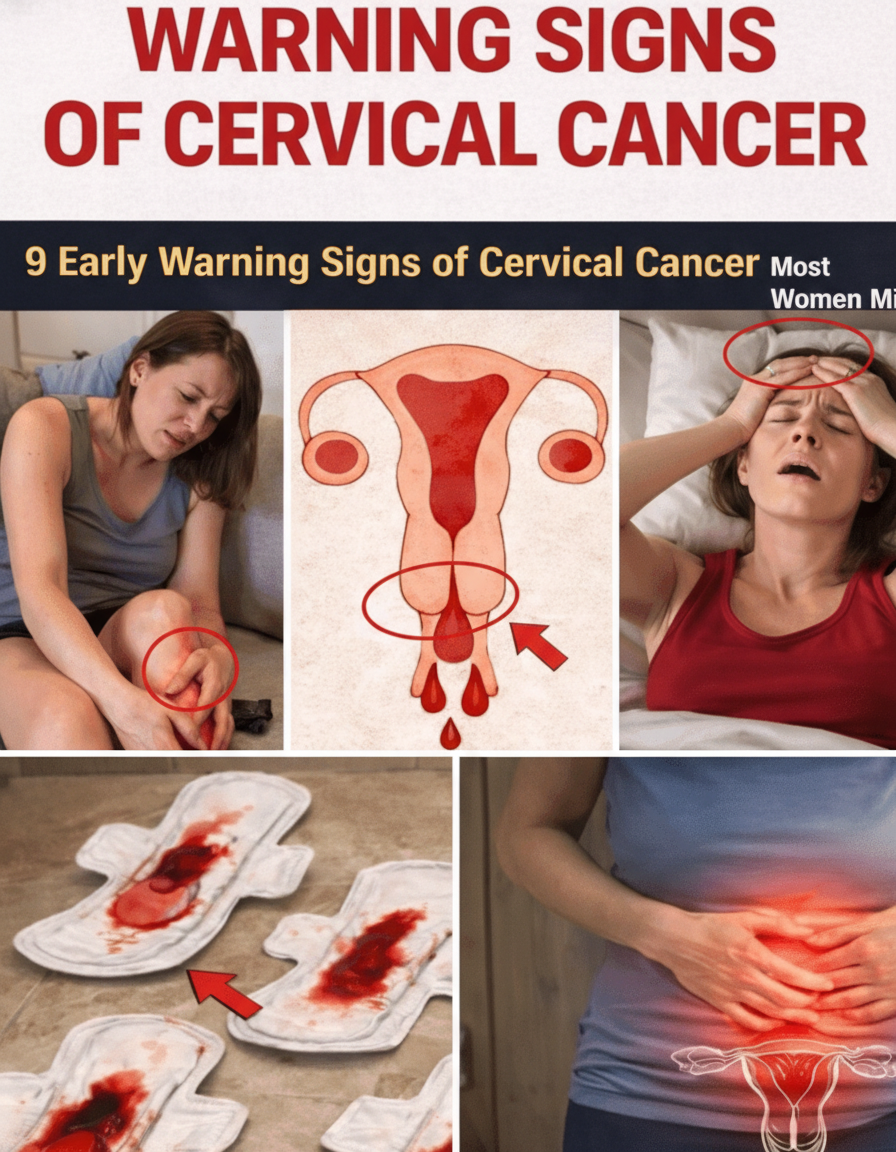
8 Key Signs of Cervical Cancer Women Should Watch For
Drawing upon insights from reputable health organizations such as the CDC, Mayo Clinic, and American Cancer Society, here are eight critical warning signs of cervical cancer to be aware of. It’s vital to remember that these symptoms can also arise from numerous non-cancerous conditions. However, their persistence, worsening, or appearance in combination should always prompt a thorough medical evaluation.
- Unusual Vaginal Discharge: Any notable alteration in vaginal discharge—such as it becoming watery, tinged with pink or brown, bloody, or developing a foul odor—can serve as an early indicator. While normal discharge varies throughout the menstrual cycle, a persistent change that deviates from your personal baseline should not be dismissed. Although infections are a common cause, ongoing atypical discharge warrants professional medical advice.
- Abnormal Vaginal Bleeding: This is frequently cited as one of the most significant red flags. Experiencing spotting or bleeding between menstrual periods, post-intercourse bleeding, any bleeding after menopause, or periods that are unusually heavy or prolonged, should immediately trigger a consultation with your doctor. Many women mistakenly attribute such bleeding to stress or hormonal shifts, but it is crucial to investigate and rule out any serious underlying conditions.
- Pain During Intercourse (Dyspareunia): Experiencing discomfort or pain during sexual activity, medically termed dyspareunia, can be a symptom of cervical changes. While it might feel awkward or embarrassing to discuss, healthcare providers are accustomed to hearing about this issue. Openly communicating such symptoms is a proactive and intelligent step for your health.
- Persistent Pelvic or Lower Back Pain: A chronic ache or discomfort in the lower abdomen, pelvis, hips, or lower back shouldn’t simply be attributed to everyday life. As cervical abnormalities advance, they can exert pressure on nearby tissues or nerves, leading to persistent pain. Consider this your body’s gentle yet firm reminder that it’s time for a medical check-up.
- Persistent Fatigue and Weakness: Do you feel utterly exhausted despite getting adequate rest? Ongoing blood loss due to abnormal bleeding can often lead to anemia, which severely depletes energy levels. While fatigue alone isn’t a definitive diagnostic tool, when combined with other suspicious signs, it acts as a critical signal to seek further investigation.
- Unexplained Weight Loss or Loss of Appetite: Losing weight without any intentional effort, particularly when accompanied by other symptoms, can signify that your body is under considerable stress. In advanced stages, cervical changes might influence metabolism or suppress appetite. Never ignore sudden, unexplained shifts in your weight or eating habits.
- Leg Swelling: Swelling in one or both legs, especially if its cause is unclear, can occur if more advanced cervical changes begin to impact blood or lymph flow. Many individuals might assume this is merely due to daily activities, but persistent or unexplained leg edema requires a thorough medical evaluation.
- Changes in Bladder or Bowel Habits: As cervical cancer progresses, it can press on the bladder or rectum. This might manifest as more frequent urination, painful urination, blood in urine, difficulty passing stool, or blood in stool. Any new and persistent changes in your urinary or bowel patterns warrant a discussion with your healthcare provider.
The Most Overlooked Clue: Persistent High-Risk HPV
Beyond the observable symptoms, there’s a crucial, often silent, underlying factor many women overlook: persistent infection with high-risk strains of Human Papillomavirus (HPV). The vast majority of cervical cancers are rooted in long-term HPV infections, and remarkably, you can harbor these infections without experiencing any noticeable symptoms. This fundamental truth underscores why routine HPV testing and Pap smears are revolutionary in preventative healthcare. These screenings are designed to identify precancerous cellular changes well before any physical signs or symptoms emerge, offering a critical window for early intervention. Extensive research consistently demonstrates that both HPV vaccination and regular screening protocols significantly diminish the risk of developing cervical cancer. It’s also important to acknowledge that many of the symptoms listed above can mimic those of less severe conditions, such as uterine fibroids, various infections, or hormonal imbalances. Therefore, the absolute key to early detection and effective management is to diligently pay attention to what feels unusual for you.
Practical Steps to Protect Your Health
Empowering yourself with knowledge about cervical cancer symptoms is the first step, but proactive health management goes further. Here’s how you can actively protect your health:
- Prioritize Regular Screenings: Adhere to your gynecologist’s recommendations for routine Pap tests and HPV screenings. These are your most powerful tools for detecting precancerous changes early.
- Consider HPV Vaccination: If you are within the recommended age range, discuss HPV vaccination with your doctor. It offers robust protection against the strains that cause most cervical cancers.
- Practice Safe Sex: While condoms don’t offer 100% protection against HPV, they can reduce the risk of transmission.
- Avoid Smoking: Smoking significantly increases the risk of cervical cancer in women with HPV. Quitting can dramatically improve your overall health and reduce your risk.
- Listen to Your Body: Pay close attention to any persistent or unusual changes, and don’t hesitate to consult a healthcare professional. Early communication can make all the difference.
Your health is invaluable. By staying informed, proactive, and attuned to your body’s signals, you can significantly reduce your risk and ensure prompt care should any concerns arise.