Cervical Cancer: 8 Critical Warning Signs to Watch For and Why Early Detection is Key
Many women experience various bodily changes throughout their lives, often attributing them to typical factors like stress, aging, or hormonal fluctuations. However, some persistent or unusual alterations could signal a more serious underlying health issue. Cervical cancer, in particular, tends to develop gradually and may not present noticeable symptoms in its initial stages. This silent progression underscores the paramount importance of recognizing and acting upon any unusual or lasting changes.
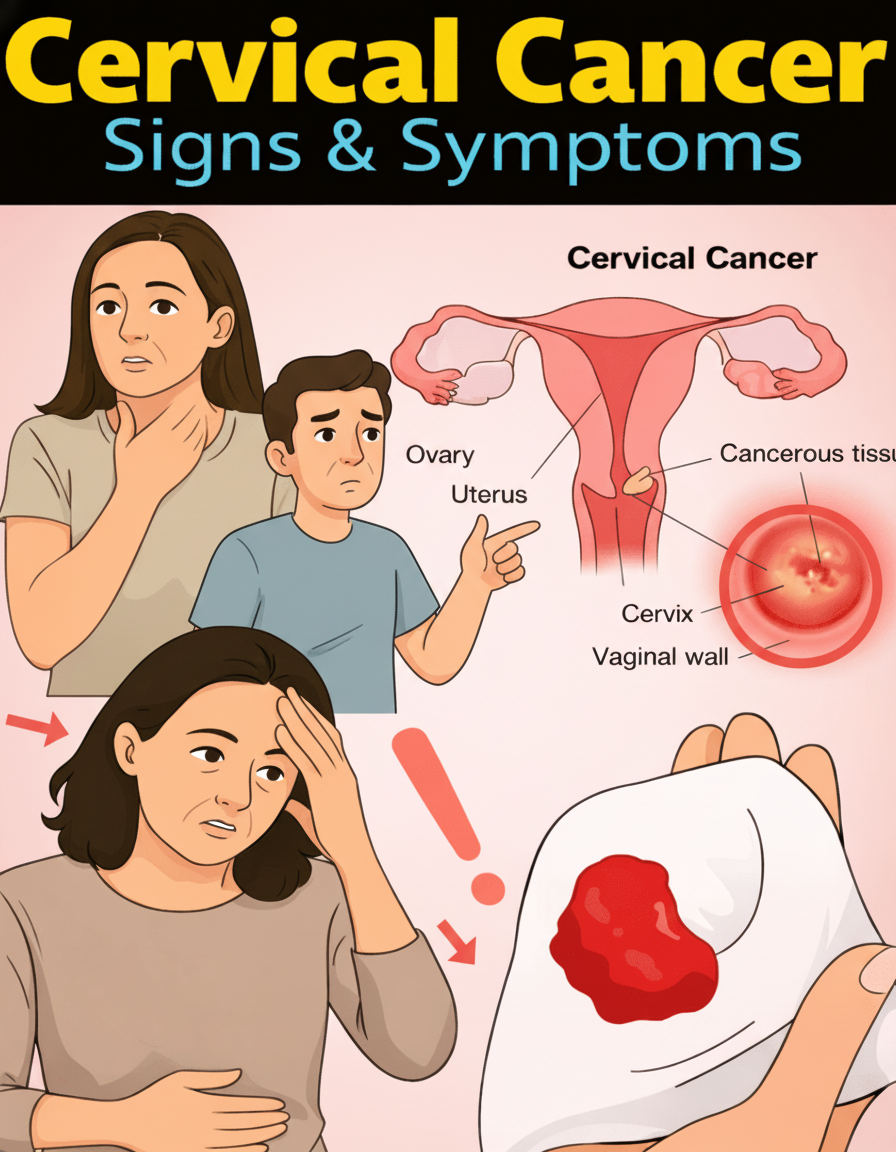
This condition originates in the cervix – the narrow, lower portion of the uterus that connects to the vagina. The vast majority of cases are linked to a prolonged infection with the Human Papillomavirus (HPV), as highlighted by leading health organizations such as the American Cancer Society and the CDC. Fortunately, routine screenings are highly effective in identifying precancerous changes early on, when they are most treatable and manageable.
Below, we delve into 8 common warning signs of cervical cancer that warrant immediate discussion with your healthcare provider. Additionally, we’ll explore essential prevention strategies and crucial next steps to safeguard your health.
Understanding Key Symptoms to Monitor
It’s important to remember that these signs are not exclusively indicative of cervical cancer; many can be caused by less serious conditions. However, if they are new, unusual, or persist over time, they absolutely deserve professional medical evaluation.
- Irregular Vaginal Bleeding: One of the most frequently reported indicators is bleeding that occurs outside of your regular menstrual cycle, after sexual intercourse, or following menopause. This can manifest as light spotting or a heavier flow, and should never be dismissed as a minor occurrence.
- Unusual Vaginal Discharge: Pay attention to any significant changes in vaginal discharge. This includes discharge that becomes watery, unusually thick, persistent, or has an unpleasant odor. While various factors can cause such changes, ongoing alterations warrant medical assessment.
- Persistent Pelvic Discomfort or Pain: An ongoing ache or pressure in the pelvic region, lower abdomen, or back that doesn’t subside could sometimes be associated with more advanced stages of cervical cancer or other conditions affecting nearby areas.
- Discomfort During Intercourse: Pain or a general sense of unease or discomfort during sexual activity is a symptom reported by many women. This signal should not be ignored and merits a conversation with a doctor.
- Unexplained Persistent Fatigue: Feeling unusually tired, weak, or lacking energy without a clear reason might accompany advancing conditions. This can often be linked to anemia, which may result from chronic bleeding, or the body’s general strain in fighting illness.
- Unintentional Weight Loss: Losing weight without making any dietary or lifestyle changes, particularly when accompanied by a reduced appetite, can be a non-specific yet significant red flag for various health issues, including certain cancers.
- Leg Swelling or Pain: In some instances, as cervical cancer progresses, it can put pressure on nearby nerves or blood vessels. This pressure may lead to swelling, discomfort, or pain in one or both legs.
- Urinary or Bowel Changes: While less common in the very early stages, as the condition advances, it might affect nearby organs. This could manifest as increased urinary urgency, frequent urination, difficulty passing urine or stool, or changes in bowel habits.
Here’s a concise overview of these crucial indicators:
| Sign | Common Presentation | Significance |
|---|---|---|
| Abnormal Bleeding | Between periods, after sex, or post-menopause | Often among the earliest noticeable indicators requiring attention. |
| Unusual Discharge | Persistent, watery, or strong-smelling | May suggest irritation, infection, or more serious underlying issues. |
| Pelvic Pain | Ongoing ache in lower abdomen or back | Could signal involvement of the cervix or surrounding structures. |
The Indispensable Role of Screening and Early Detection
Cervical cancer stands out as one of the most preventable cancers, largely due to the effectiveness of routine screening methods like Pap tests and HPV screening. These crucial tests are designed to identify abnormal cell changes or the presence of high-risk HPV types before they develop into serious cancerous conditions. Health organizations typically recommend starting these screenings around age 21 and continuing them regularly according to specific guidelines.
Proactive Steps for Prevention
Adopting certain lifestyle choices and health habits can significantly reduce your risk of developing cervical cancer:
- Consider HPV Vaccination: The HPV vaccine is a powerful tool for prevention and is available for individuals across a wide age range. Discuss with your healthcare provider if vaccination is appropriate for you.
- Attend Regular Screenings: Adhere to the recommended schedule for Pap tests and HPV screenings. Consistent screening is vital for catching precancerous changes early.
- Practice Safer Sex: Using barrier methods like condoms can help reduce the risk of HPV transmission, although it doesn’t offer complete protection.
- Avoid Smoking: Smoking has been identified as a risk factor that can weaken the immune system and make women more susceptible to HPV infection and its progression to cervical cancer.
Final Thoughts: Empowering Your Health Journey
Being aware of these common warning signs empowers you to take control of your health and seek timely medical attention. If you notice anything unusual, persistent, or concerning about your body – especially any of the changes mentioned above – do not hesitate. Reach out to a qualified healthcare professional promptly for personalized guidance, thorough examination, and accurate diagnosis. Early detection through vigilant self-awareness and professional care is truly your best defense.
Frequently Asked Questions
- When should I consult a doctor about these symptoms?
- Any new, persistent, or worsening change in your body, particularly any of the signs discussed, warrants an immediate medical consultation. There’s no need to wait for multiple symptoms to appear.
- How often should I undergo cervical cancer screenings?
- Guidelines, such as those from the U.S. Preventive Services Task Force (USPSTF), suggest Pap tests every three years starting at age 21, or a combination of Pap and HPV co-testing at longer intervals (e.g., every five years) for women over 30.
- Is the HPV vaccine still beneficial for adults?
- Yes, absolutely. The HPV vaccine is approved for adults up to age 45, and for some, even beyond. A discussion with your healthcare provider can clarify if vaccination is recommended for your specific situation and age.
Disclaimer: This article is provided for general informational purposes only and should not be considered as medical advice. It is not intended to diagnose, treat, cure, or prevent any disease. The information presented is compiled from reputable sources such as the American Cancer Society, CDC, and Mayo Clinic. Always consult a qualified healthcare professional for any personal health concerns, medical screenings, or treatment recommendations. Timely and professional medical care is crucial for early detection and effective management of any health condition.