You’re folding laundry late at night when you notice light spotting that doesn’t align with your cycle. It’s not painful, so you brush it off as stress or hormones—something many women do. But these subtle changes can be early clues to cervical cancer, a disease that affects thousands in the U.S. each year. Research from trusted sources like the American Cancer Society shows that while cervical cancer is highly preventable with screening, many cases advance because early signs go unnoticed. The good news? Recognizing these whispers from your body and acting promptly can make all the difference—often catching issues before they become serious.
There’s one key habit that turns awareness into protection, and we’ll reveal it toward the end—along with how simple steps today can dramatically shift your future health story.

Why Cervical Cancer Often Goes Unnoticed Until Later Stages
Cervical cancer develops slowly, usually from persistent infection with high-risk strains of human papillomavirus (HPV), a common virus spread through intimate contact. Studies indicate that HPV infections can linger silently for years, allowing abnormal cells to form without obvious pain or drama. By the time more noticeable symptoms appear, the condition may require more intensive management.
Busy lives make it easy to dismiss subtle shifts. Careers, family, and daily demands push personal health lower on the list. Yet organizations like the Mayo Clinic and CDC emphasize that early changes are often mild and easy to rationalize—exactly when detection and intervention work best. The key is tuning in before things escalate.
The Subtle Way Early Signs Appear
Early cervical cancer rarely “screams.” Instead, it whispers through small disruptions in your normal patterns. These changes might come and go, feel minor, or seem tied to everyday factors like stress or age. But here’s the truth: your body knows its baseline. When something feels persistently “off,” it’s worth paying attention.
But that’s not all—let’s break down the most commonly overlooked signs, backed by expert insights from leading health authorities.

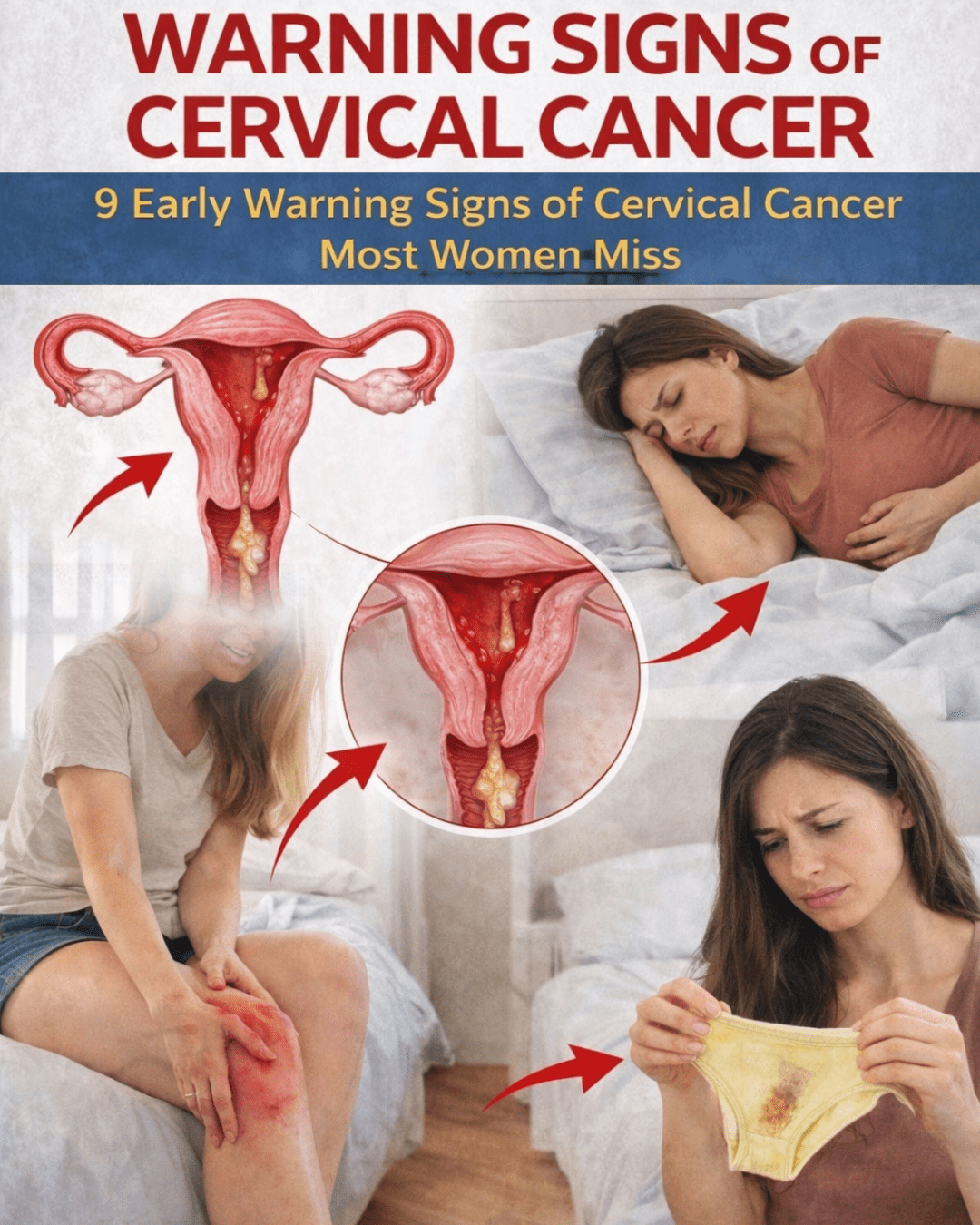
Sign 1: Abnormal Vaginal Bleeding That Feels “Off”
Unexpected bleeding tops the list of early indicators. This includes spotting between periods, after intercourse, or heavier flows than usual.
Many women, like one 38-year-old who noticed post-intimacy spotting, initially attribute it to fatigue or hormones. When it persisted, evaluation caught precancerous changes early. Abnormal bleeding warrants prompt attention—it’s one of the clearest signals something may need checking.
Sign 2: Unusual Vaginal Discharge
Changes in discharge—watery, pinkish, bloody, thick, or with an unusual odor—can feel awkward to discuss. Yet this is a frequent early clue.
Women often self-treat assuming a minor infection. Persistent shifts, however, may reflect cervical tissue changes. If your normal discharge pattern alters noticeably and lingers, it’s a prompt to seek professional input.
Sign 3: Pain or Discomfort During Intercourse
Intimacy should feel comfortable. Pain, pressure, or new discomfort during or after sex isn’t something to endure or blame on dryness alone.
One woman in her late 30s avoided closeness due to this issue, only to discover treatable changes upon evaluation. Discomfort here is valuable information—don’t power through it.

Sign 4: Persistent Pelvic Pain or Pressure
A dull ache, heaviness, or ongoing pressure in the lower abdomen often gets blamed on posture, work, or monthly cycles.
When it lingers or worsens, it may signal pelvic involvement. Rating your daily pelvic comfort helps track whether it’s transient or persistent—anything ongoing deserves curiosity.
Sign 5: Longer or Heavier Menstrual Periods
Sudden shifts in your cycle—periods lasting longer, flowing heavier, or leaving you more drained—can point to underlying changes.
Tracking even for a few months reveals patterns memory might miss. Many women normalize increasing fatigue during cycles, but trends matter.
Sign 6: Bleeding After Menopause
Any vaginal bleeding post-menopause, even light spotting, is never normal and should be evaluated right away.
Postmenopausal bleeding prompted one woman in her 50s to act quickly—leading to early intervention. This sign is particularly urgent.
Sign 7: Unexplained Fatigue or Weakness
Constant tiredness without clear cause can accompany other symptoms. While fatigue has many origins, when paired with reproductive changes, it adds context.
Listen to your energy levels—they’re part of the bigger picture.

Sign 8: Leg Pain or Swelling
Less common early on, but persistent or one-sided leg discomfort/swelling can occur if pelvic pressure affects nearby structures.
New or ongoing changes here, especially alongside other signs, merit note.
Sign 9: Changes in Urination or Bowel Habits
Frequent urges, difficulty emptying the bladder, or bowel pattern shifts may stem from pelvic pressure.
Often attributed to age or diet, these warrant attention when combined with other clues.
Quick Reference: Common Early Warning Signs
- Abnormal bleeding (between periods, after sex, post-menopause)
- Unusual vaginal discharge (watery, bloody, foul-smelling)
- Pain during intercourse
- Persistent pelvic pressure or pain
- Heavier/longer periods
- Post-menopausal bleeding
- Unexplained fatigue
- Leg pain/swelling
- Urinary/bowel changes
These signs can stem from non-cancer causes too—that’s why professional evaluation is essential.
Prevention and Early Action: Steps You Can Take Right Now
Cervical cancer links strongly to HPV, and prevention focuses on vaccination and screening. Regular checks detect precancerous changes long before symptoms arise.
Here’s a clear overview of current screening recommendations (based on guidelines from the American Cancer Society and others):
- Ages 21–29: Pap test every 3 years
- Ages 30–65: HPV test alone every 5 years, or Pap + HPV co-testing every 5 years (or Pap every 3 years if HPV not available); self-collection HPV options now available for many
- Over 65: Discuss with your provider—may stop if prior tests normal
Prevention Tips Checklist
- Get the HPV vaccine if eligible (ideally before exposure)
- Schedule regular screenings as recommended
- Avoid smoking, which weakens immune response to HPV
- Practice safe intimate habits
- Pay attention to body changes and seek care promptly
Acting early shifts outcomes dramatically—many precancers resolve with simple treatment.
Imagine the Peace of Mind a Month from Now
Picture scheduling that overdue screening, noting any changes, and gaining clarity. Whether results reassure or guide next steps, you’re no longer wondering. Early awareness replaces uncertainty with control—and potentially protects your life.
If this resonates, share it with a woman you care about. Awareness multiplies protection.
Frequently Asked Questions (FAQ)
What is the number one early sign of cervical cancer?
Abnormal vaginal bleeding, such as between periods or after intercourse, is among the most reported early indicators—though many have no symptoms initially.
Can cervical cancer be prevented?
Yes—largely through HPV vaccination and regular screening, which catch changes before cancer develops.
How often should I get screened for cervical cancer?
Guidelines vary by age: typically Pap every 3 years (21-29) or HPV-focused every 5 years (30-65). Consult your provider for personalized advice.
This article is for informational purposes only and is not a substitute for professional medical advice. Always consult a qualified healthcare provider about symptoms, screening, or any health concerns.