Empowering Health: Understanding Cervical Cancer, Its Warning Signs, and The Life-Saving Power of Early Detection
Cervical cancer originates in the cells of the cervix, which is the lower, narrow end of the uterus connecting to the vagina. Remarkably, it stands as one of the most preventable and highly treatable forms of cancer, especially when identified at an early stage. This success is largely attributed to effective screening methods, such as Pap smears and HPV testing, alongside the protective HPV vaccine. The predominant cause behind the vast majority of cervical cancer cases is a persistent infection with high-risk types of the Human Papillomavirus (HPV). HPV is a widespread virus transmitted through skin-to-skin sexual contact. While most HPV infections resolve naturally, in certain individuals, the virus can linger for years, gradually leading to abnormal cellular changes that may progress into cancer if left undiagnosed and untreated.
The Life-Saving Impact of Early Detection
The stage at which cervical cancer is diagnosed critically influences treatment outcomes and survival rates. Early detection dramatically improves a woman’s prognosis:
- When cervical cancer is identified at a localized stage (meaning it is contained solely within the cervix), the 5-year survival rate exceeds 91–93%.
- If the cancer has spread regionally (to nearby tissues or lymph nodes), the survival rate typically decreases to approximately 58–60%.
- In cases where the disease is distant (metastatic, having spread to other parts of the body), the 5-year survival rate drops significantly to around 17–19%.
Crucially, consistent cervical screening plays a pivotal role by identifying pre-cancerous changes, such as dysplasia or Cervical Intraepithelial Neoplasia (CIN), years before they can evolve into invasive cancer. These pre-cancerous lesions are nearly always treatable and curable through straightforward outpatient procedures, including LEEP (Loop Electrosurgical Excision Procedure), cryotherapy, or cone biopsy.
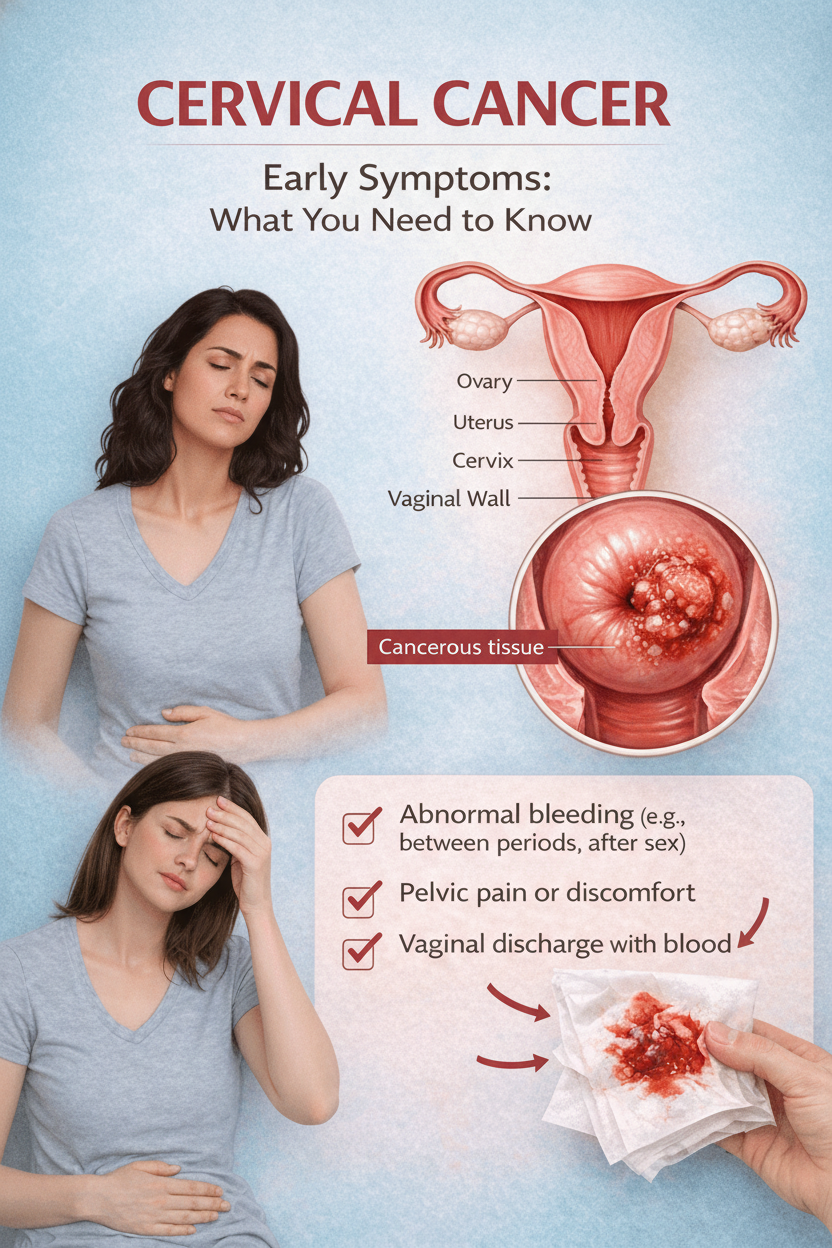
Key Warning Signs and Symptoms of Cervical Cancer
It’s crucial to understand that early-stage cervical cancer and pre-cancerous conditions frequently present no noticeable symptoms. This asymptomatic nature underscores the critical importance of regular screening. When symptoms do emerge, they often indicate that the disease has advanced beyond its very initial stages. Be vigilant for these potential indicators:
1. Abnormal Vaginal Bleeding
This is often the most common and significant early warning sign of cervical cancer.
- Bleeding occurring between menstrual periods.
- Bleeding after sexual intercourse.
- Any instance of bleeding post-menopause, regardless of how slight, is considered abnormal and warrants immediate medical attention.
- Menstrual periods that become unusually long or notably heavier than your typical cycle.
2. Unusual Vaginal Discharge
- Discharge that is watery, contains blood, or has a foul odor.
- Any persistent discharge that deviates significantly from your normal pattern in terms of color, consistency, or smell.
3. Pain During or After Sexual Intercourse (Dyspareunia)
Experiencing discomfort or pain during or following sexual activity can be a symptom.
4. Pelvic Pain or Discomfort
- A dull ache or sharp pain located in the lower abdomen or pelvis that is distinct from typical menstrual cramps.
5. Persistent Pain in the Lower Back or Legs
- Particularly concerning if the pain is continuous, affects only one side, and intensifies over time, as this could suggest the cancer has spread to lymph nodes or nerves.
6. Unexplained Weight Loss or Loss of Appetite
- These symptoms are more commonly observed in the advanced stages of cervical cancer.
7. Persistent Fatigue or Weakness
- Often a consequence of anemia, which can result from chronic blood loss associated with the cancer.
8. Swelling in One or Both Legs
- Typically a later-stage symptom, caused by a tumor exerting pressure on pelvic veins or lymph nodes.
Factors Increasing Your Risk of Cervical Cancer
While cervical cancer can affect any woman, certain factors significantly elevate the risk. Understanding these can help you discuss appropriate screening and preventive measures with your healthcare provider:
- Persistent High-Risk HPV Infection: The most significant risk factor. Specific types, notably HPV 16 and 18, are implicated in approximately 70% of all cervical cancer cases.
- Infrequent or Absent Cervical Screening: A lack of regular Pap tests and HPV screening prevents the early detection of pre-cancerous changes.
- Smoking: Tobacco use has been shown to double the risk of developing cervical cancer.
- Compromised Immune System: Conditions that weaken the immune system, such as HIV infection, prolonged use of corticosteroids, or organ transplantation, make it harder for the body to clear HPV infections.
- Multiple Sexual Partners or Early Age at First Intercourse: These factors increase exposure to HPV.
- Long-Term Oral Contraceptive Use: A minor increase in risk has been observed with the use of oral contraceptives for five years or longer.
- Multiple Full-Term Pregnancies: A slight increase in risk is noted after three or more full-term pregnancies.
The Mechanics of Early Detection: How Screening Saves Lives
The cornerstone of preventing cervical cancer and improving survival rates lies in robust early detection strategies. Here’s how these vital tools work to identify and address potential issues long before they become life-threatening:
- HPV Test: This advanced screening method specifically identifies the presence of high-risk HPV strains, which are the primary cause of cervical cancer. It can detect the virus even before any abnormal cellular changes have developed.
- Pap Smear (Pap Test): A Pap smear involves collecting cells from the cervix to examine them for any abnormal changes, such as dysplasia or Cervical Intraepithelial Neoplasia (CIN). This test can pinpoint pre-cancerous cells years before they might progress into invasive cancer.
- Colposcopy and Biopsy: If a Pap smear or HPV test returns abnormal results, a colposcopy is performed. This procedure uses a magnifying instrument to examine the cervix more closely. During a colposcopy, a biopsy (taking a small tissue sample) may be conducted to allow for a precise diagnosis and to guide early treatment decisions.
- Treatment Procedures (LEEP, Cone Biopsy, Cryotherapy): Should pre-cancerous tissue be identified (e.g., CIN 2–3), various outpatient procedures are available to remove these abnormal cells effectively. Techniques like Loop Electrosurgical Excision Procedure (LEEP), cone biopsy, or cryotherapy boast a cure rate exceeding 90–95% for high-grade pre-cancers, preventing them from developing into full-blown cancer.
General Cervical Cancer Screening Guidelines (as of 2025)
Adhering to recommended screening schedules is paramount for cervical cancer prevention. These are general guidelines, and your healthcare provider will tailor recommendations based on your individual health history:
- Ages 21–29: A Pap smear is recommended every three years.
- Ages 30–65: You have several options:
- Co-testing with both a Pap smear and an HPV test every five years.
- An HPV test alone every five years.
- A Pap smear alone every three years.
- After Age 65: Screening can typically cease if you have a history of normal screening results for the past 10 years and no prior history of high-grade cervical lesions.
- For Higher-Risk Individuals: Women with specific risk factors, such as HIV infection, immunosuppression, or a history of CIN 2 or higher, will likely require more frequent and personalized screening schedules.
The Bottom Line: Cervical Cancer is Highly Preventable
To reiterate, cervical cancer stands out as one of the most preventable forms of cancer. This remarkable preventability is due to several critical factors:
- Known Cause: We have a clear understanding of its primary cause – persistent infection with high-risk strains of Human Papillomavirus (HPV).
- Effective Screening: Highly effective screening tools are available that can identify cellular changes years before they progress into invasive cervical cancer.
- Treatable Pre-Cancers: Pre-cancerous changes are not only detectable but also highly treatable through relatively minor medical procedures, effectively stopping the disease in its tracks.
The unfortunate reality is that the vast majority of cervical cancer fatalities occur among women who have either never undergone screening or have not maintained a regular screening schedule. This highlights the immense power of proactive healthcare.
Your Empowering Action Step
Every woman has the power to protect her health against cervical cancer. Here’s what you can do:
- Check Your Screening History: Determine the date of your last Pap test or HPV screening. If more than 3 to 5 years have passed (contingent on your age and individual risk factors), make it a priority to schedule your next screening appointment this month.
- Act on Warning Signs: If you experience any of the previously mentioned warning signs – particularly abnormal vaginal bleeding or persistent unusual discharge – consult a gynecologist without delay, even if your most recent screening was normal.
Remember, prioritizing early detection transforms a potentially life-threatening diagnosis into a condition that is, in almost all cases, highly curable.
Disclaimer
Please note: The information provided in this article is intended solely for general informational purposes and should not be considered as medical advice. Any concerning symptoms, such as abnormal vaginal bleeding, persistent unusual discharge, pelvic pain, or any other health changes, warrant a prompt consultation with a qualified healthcare professional for proper diagnosis and personalized guidance.