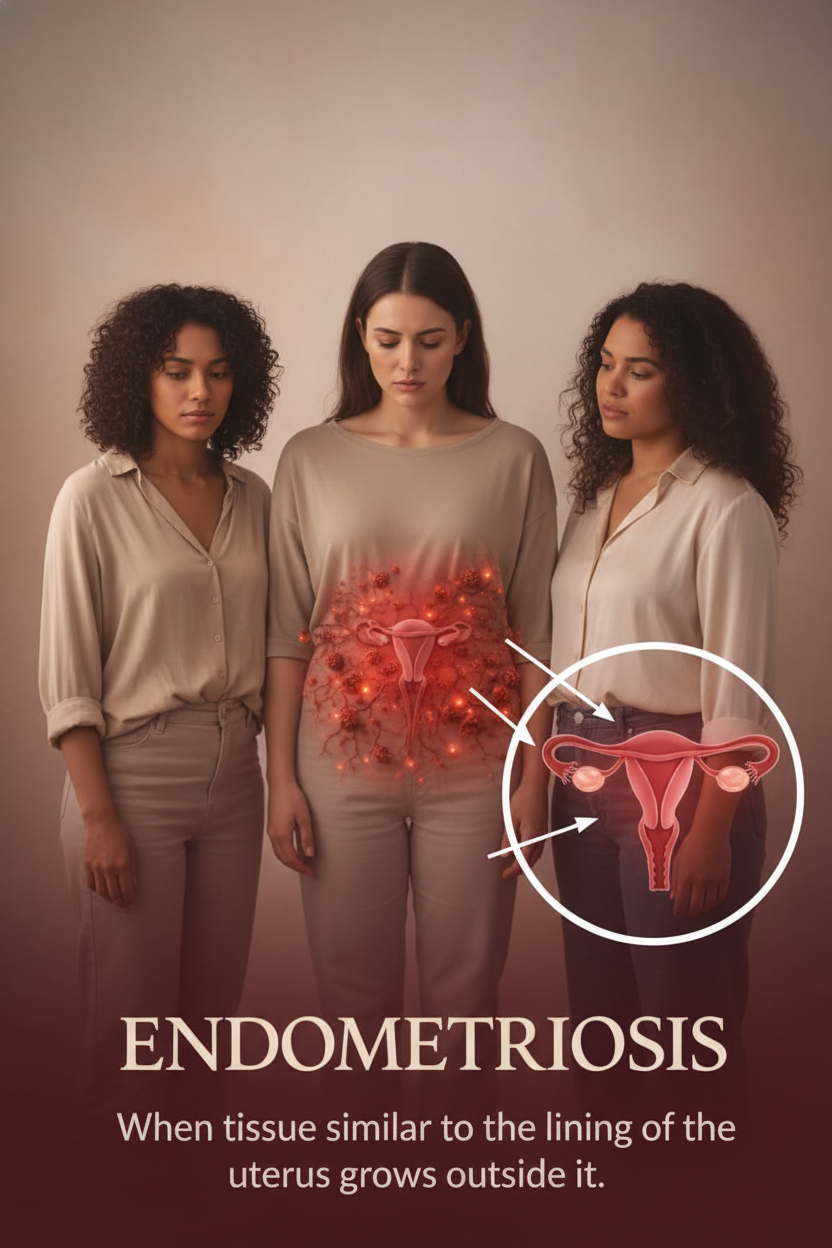
Understanding Endometriosis: A Comprehensive Guide for Women on Symptoms, Causes, and Effective Management
Endometriosis is a prevalent chronic condition impacting approximately 1 in 10 women globally during their reproductive years, affecting around 190 million individuals worldwide. This condition often manifests with debilitating pain and significant challenges to fertility. Despite its widespread impact, many women endure an average diagnostic delay of 7-10 years, primarily because symptoms are frequently dismissed as ‘normal period pain’ or attributed to other unrelated issues.
Characterized by the growth of tissue similar to the uterine lining (endometrium) outside the uterus, endometriosis can lead to chronic inflammation, scarring, and adhesions. Early recognition and understanding of this condition are crucial for better disease management and a significantly improved quality of life. This guide offers a clear, concise overview based on reputable sources such as the World Health Organization (WHO), Mayo Clinic, and Cleveland Clinic.
Common Symptoms: Frequently Overlooked or Misdiagnosed
The presentation and severity of endometriosis symptoms can vary significantly; some individuals may experience extensive disease with minimal discomfort, while others suffer intensely from limited endometrial growths. Awareness of these often-misunderstood signs is vital.
| Symptom Description | Why It’s Often Ignored or Misinterpreted |
|---|---|
| Excruciating Period Pain (Dysmenorrhea): Intense, debilitating cramps that extend far beyond typical menstrual discomfort. | Frequently dismissed as simply ‘heavy periods’ or a ‘normal part of menstruation’ that women must endure. |
| Persistent Pelvic Pain: Ongoing discomfort in the lower abdomen and/or back, not limited to menstrual cycles. | Often attributed to everyday stress, muscle strain, or other general aches. |
| Pain During or After Sexual Intercourse (Dyspareunia): Deep-seated discomfort experienced during or following sexual activity. | Often assumed to be unrelated to a specific medical condition, or considered a normal variation. |
| Heavy or Irregular Menstrual Bleeding: Experiencing excessive blood flow, prolonged periods, or spotting between cycles. | Commonly explained away as hormonal imbalances or other benign menstrual irregularities. |
| Infertility or Difficulty Conceiving: Challenges in becoming pregnant despite regular, unprotected intercourse. | Often ascribed to age, general reproductive health issues, or other unrelated factors. |
| Gastrointestinal Issues: Symptoms like bloating, diarrhea, or constipation, particularly worsening during menstruation. | Frequently misdiagnosed as Irritable Bowel Syndrome (IBS) or attributed solely to dietary factors. |
| Chronic Fatigue: Persistent and overwhelming tiredness that doesn’t improve with rest. | Often dismissed as a consequence of a busy lifestyle, aging, or general exhaustion. |
| Other Symptoms: These may include painful bowel movements, discomfort during urination, and nausea. | These can often be mistaken for symptoms of other conditions, delaying an accurate endometriosis diagnosis. |
Understanding Causes and Risk Factors
While the precise etiology of endometriosis remains elusive, several prominent theories attempt to explain its development:
- Retrograde Menstruation: This theory suggests that during menstruation, menstrual blood containing endometrial cells flows backward through the fallopian tubes into the pelvic cavity instead of exiting the body.
- Immune System Dysfunction: A compromised immune system may fail to recognize and destroy endometrial-like tissue growing outside the uterus.
- Genetic Predisposition: There is evidence of a familial link, indicating a higher risk if close relatives have endometriosis.
- Hormonal or Embryonic Cell Transformation: Cells lining the abdomen or pelvis might transform into endometrial-like cells under certain hormonal influences or during embryonic development.
Key risk factors associated with developing endometriosis include:
- Starting menstruation at an early age.
- Having short menstrual cycles (less than 27 days).
- Never having given birth.
Diagnosis and Effective Management Strategies
Currently, there is no definitive cure for endometriosis, but a range of treatments can effectively manage symptoms and improve quality of life. Early and accurate diagnosis is key to developing a personalized management plan.
Diagnostic Approaches:
- Pelvic Exam: A physical examination can sometimes reveal abnormalities like cysts or tenderness.
- Ultrasound: Imaging techniques can identify endometrial cysts (endometriomas) but may not detect all forms of the disease.
- Laparoscopy: Considered the ‘gold standard,’ this minimally invasive surgical procedure allows direct visualization and biopsy of endometrial implants.
Management Options:
- Pain Relief Medication: Non-steroidal anti-inflammatory drugs (NSAIDs) can help manage pain and inflammation.
- Hormonal Therapy: Treatments such as birth control pills (oral contraceptives), GnRH agonists, or progestins can suppress the growth of endometrial tissue and reduce pain.
- Surgical Intervention: Laparoscopic surgery can precisely remove endometrial tissue, adhesions, and cysts, often providing significant relief for severe pain or to improve fertility prospects.
- Fertility Support: For women struggling with conception due to endometriosis, assisted reproductive technologies (ART) like IVF may be recommended.
- Lifestyle Adjustments: Adopting an anti-inflammatory diet, engaging in regular exercise, and practicing stress reduction techniques can complement medical treatments and enhance overall well-being.
With appropriate diagnosis and management, many individuals with endometriosis can lead fulfilling and well-controlled lives.
The Crucial Role of Awareness
Endometriosis significantly impacts various aspects of a woman’s life, including professional productivity, personal relationships, and mental health. The common delay in diagnosis, often stemming from the normalization of chronic pain, exacerbates these challenges. It is imperative for women to advocate for themselves and speak up if they experience persistent or unusual symptoms. Seeking early medical evaluation from a gynecologist specializing in endometriosis is paramount, as timely intervention can profoundly improve outcomes and prevent long-term complications.
Disclaimer: This information is provided for educational purposes only and should not be considered medical advice. Endometriosis symptoms can vary widely; therefore, it is essential to consult with a qualified gynecologist for accurate diagnosis and personalized treatment recommendations. Early medical attention is crucial for effective management. Individual results from treatments may vary.