Many women experience subtle changes in their breasts and dismiss them as normal fluctuations from hormones, stress, or everyday life. It’s easy to think these shifts are harmless and will resolve on their own, especially with busy schedules pulling attention elsewhere. But ignoring them can be risky, as some changes signal the early stages of breast cancer, allowing a highly detectable condition to advance when early action could make all the difference. The encouraging truth? Early detection dramatically improves outcomes—and I’ll show you exactly what to watch for, plus a simple plan to stay ahead.
But that’s not all… there’s one often-overlooked sign that could indicate spread already, revealed toward the end.

Why Paying Attention to Breast Changes Matters
Breast cancer doesn’t always announce itself loudly. It often starts quietly in the milk ducts or lobules, without clear symptoms at first.
Research from the American Cancer Society shows that when detected early—while still localized to the breast—the 5-year relative survival rate reaches nearly 99%. That’s powerful evidence that awareness and prompt checks save lives.
In 2025, an estimated 316,950 new cases of invasive breast cancer are expected in women in the U.S., plus about 2,800 in men. Yet over 4 million survivors today prove early intervention works.
The reality is, many delays stem from waiting it out. Knowledge flips that script.
Here’s the interesting part: Men can develop breast cancer too, though it’s rarer. Everyone should know these signs.
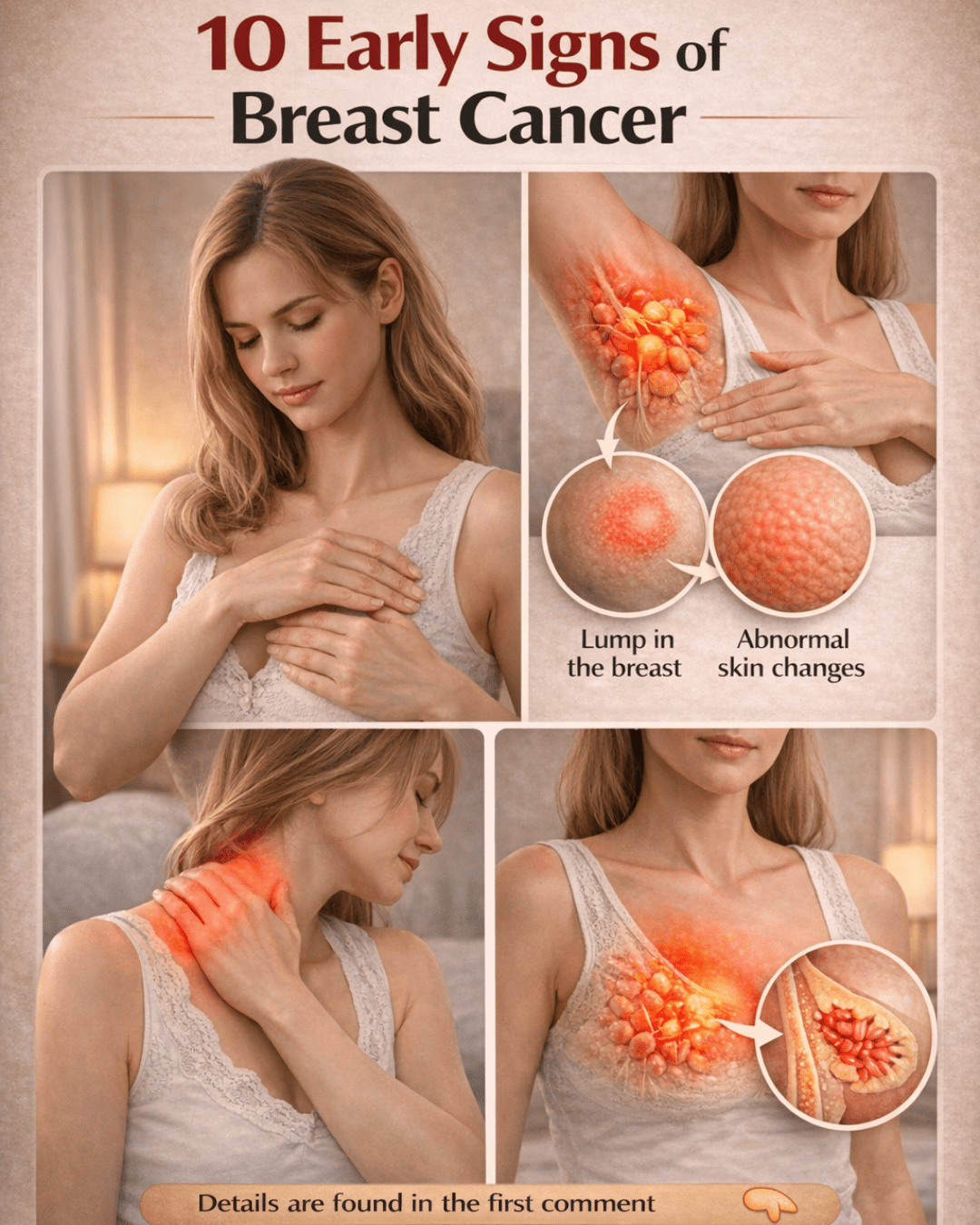
10 Key Warning Signs to Watch For
These changes can appear gradually or suddenly. Most breast changes are benign, but persistent ones deserve evaluation.
10. Unexplained Changes in Breast Size or Shape
One breast suddenly appearing larger, heavier, or differently shaped—without links to weight gain, pregnancy, or your cycle—warrants attention.
Red flags include:
- Affecting only one side
- Lasting more than a couple of weeks
- Accompanied by firmness or pulling sensation
Tip: Compare monthly photos in consistent lighting to spot subtle shifts over time.

9. Skin Dimpling or Texture Changes
Breast skin that looks puckered, like orange peel (peau d’orange), or dimpled can signal trouble.
This occurs when cancer cells affect lymphatic drainage, tugging the skin inward. It’s more common in aggressive types.
How to check:
- Arms relaxed at sides
- Arms raised overhead
- Hands on hips to tense muscles
- Gently press skin for tethering
New dimpling? See a doctor promptly.
8. Persistent Itching, Redness, or Rash
Itching that lingers for weeks, paired with redness, warmth, or swelling, isn’t always a simple irritation.
These can point to inflammatory breast cancer (IBC), a rare but fast-growing form making up 1-5% of cases. It’s often misdiagnosed as infection initially.
But here’s what sets it apart: Symptoms worsen quickly, affecting much of the breast.
7. A New Lump or Thickened Area
The classic sign: A hard, irregular, immovable lump, often painless.
Unlike fluid-filled cysts that move and fluctuate, these feel fixed and firm.
Not all lumps are cancer—many are benign—but any new one needs checking.

6. Persistent Pain in One Spot
Most breast pain ties to cycles or caffeine, but constant, localized ache unrelated to your period stands out.
It’s less common as an early sign, but don’t brush it off if it persists.
5. Swelling in the Breast or Armpit
Cancer doesn’t always form a distinct lump. Sometimes it causes overall breast swelling or enlarged armpit nodes.
This diffuse change can feel like fullness or heaviness on one side.
4. Nipple Turning Inward (Retraction)
A nipple that suddenly inverts, when it used to point out, is a red flag.
This happens as underlying tissue pulls it inward.
3. Changes to the Nipple or Areola Skin
Flaking, scaling, crusting, or redness around the nipple/areola may indicate Paget’s disease—a rare form linked to underlying cancer.
It resembles eczema but doesn’t improve with typical treatments.
2. Unusual Nipple Discharge
Spontaneous discharge (not from squeezing), especially bloody or clear, requires evaluation.
Milky discharge during non-breastfeeding times can also signal issues.
Bloody? Highest concern level.
1. Swollen Lymph Nodes Under the Arm or Near Collarbone
Hard, enlarged nodes here can mean cancer has begun spreading.
This is the sign that often indicates progression—don’t wait on it.

Your Breast Health Action Plan: Steps You Can Take Today
Empower yourself with these practical habits:
- Perform monthly self-exams: Lie down, use pads of fingers in circles from outer to center.
- Track changes: Use a journal or app for notes/photos.
- Schedule screenings: Annual mammograms starting at recommended age (often 40+), plus clinical exams.
- Discuss risks: Talk family history, density, or genetics with your doctor.
Higher-risk factors include:
- Age over 50
- Family history or BRCA mutations
- Dense breasts
- Prior radiation exposure
When to See a Doctor Urgently
Contact a healthcare provider right away if you notice:
- Bloody discharge + lump
- Rapid breast redness/swelling/warmth
- Fixed lump with node swelling
- Any sign lasting >2 weeks
Early evaluation leads to better options.
Conclusion: Listening to Your Body Is Empowering
Recognizing these 10 warning signs puts you in control. Many changes turn out benign, but acting swiftly ensures peace of mind—and the best possible outcome.
Share this with loved ones, prioritize your checks, and remember: Awareness isn’t fear; it’s strength.
Frequently Asked Questions
1. Can men get breast cancer?
Yes, though rare—about 2,800 cases expected in U.S. men in 2025. Signs are similar, like lumps or nipple changes.
2. At what age should I start mammograms?
Guidelines vary, but many recommend starting at 40-45 annually. Discuss personal risks with your doctor for tailored advice.
3. Are all breast lumps cancerous?
No—most are benign cysts or fibroadenomas. But any new lump should be evaluated by a professional.
Disclaimer: This article is for informational purposes only and not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider with any questions about your health or symptoms. Early detection improves outcomes, but individual cases vary.
(Word count: approximately 1,350)