Your body often sends subtle signals long before a serious health issue becomes obvious. Many women experience changes they attribute to stress, aging, or everyday life, only to later discover those were early warnings of cervical cancer. Ignoring these signs can allow the disease to progress, making it harder to manage and impacting your quality of life in profound ways.
The good news? When detected early, cervical cancer is highly treatable, with excellent outcomes for most women. But here’s the key insight many overlook: the most critical “silent” factor isn’t always a dramatic symptom—it’s something that often shows no signs at all. Keep reading to discover the eight signs you shouldn’t ignore, including that under-recognized one at the end that could change everything.

Understanding Cervical Cancer: Why Early Detection Matters
Cervical cancer develops in the cells of the cervix, the lower part of the uterus that connects to the vagina. According to reliable sources like the American Cancer Society and Mayo Clinic, nearly all cases are linked to persistent infection with high-risk types of human papillomavirus (HPV), a common virus spread through sexual contact.
Early-stage cervical cancer often produces no symptoms at all. That’s why regular screenings are so vital—they can find precancerous changes before they turn into cancer.
But as the cancer grows, symptoms may appear. Research shows that catching it early dramatically improves prognosis. Women diagnosed at an early stage have a much higher chance of successful management compared to later stages.
The truth is, no woman is immune. It most commonly affects those over 30, but younger women can be at risk too, especially with factors like smoking, multiple sexual partners, or a weakened immune system.
Here’s the interesting part: many of these warning signs mimic common issues like infections or hormonal shifts. That’s why they’re easy to dismiss—but paying attention could make all the difference.
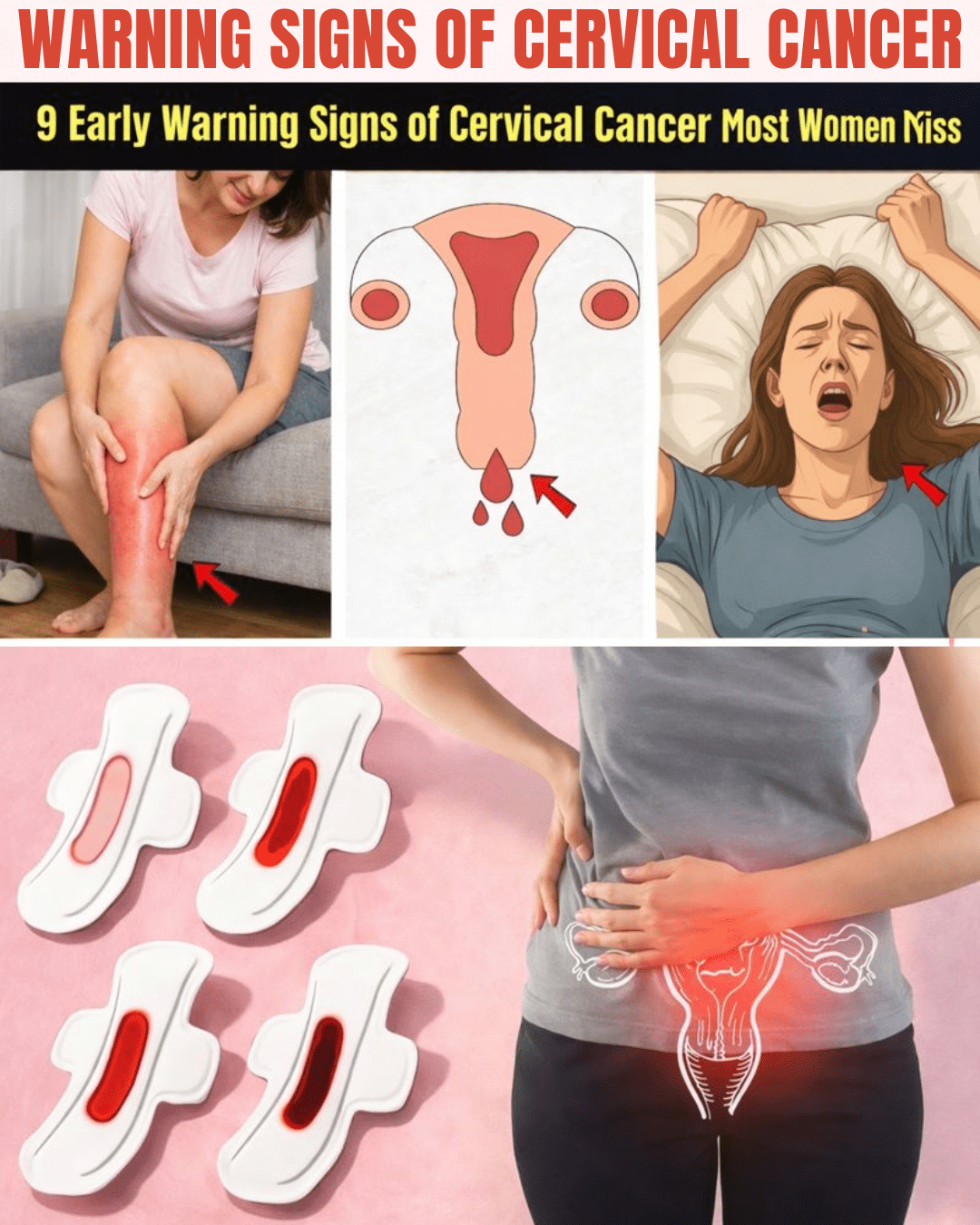
8 Key Warning Signs of Cervical Cancer
Let’s break down the signs that warrant a closer look. Remember, these can stem from other causes, but if they’re new or persistent, it’s worth discussing with your doctor.
1. Abnormal Vaginal Bleeding
This is one of the most common red flags. Bleeding between periods, after intercourse, or after menopause isn’t normal.
Many women chalk it up to irregular cycles or stress. But studies from the Mayo Clinic indicate this could signal changes in the cervix.
If you’ve noticed spotting or heavier bleeding than usual, don’t wait—get it checked.

2. Unusual Vaginal Discharge
Watery, bloody, or foul-smelling discharge that persists could be a clue.
While infections are a frequent cause, ongoing unusual discharge might point to cervical issues, per the American Cancer Society.
Track any changes in color, consistency, or odor. Your body knows what’s normal for you.
3. Pain During Intercourse
Discomfort or pain during sex, known as dyspareunia, is often overlooked due to embarrassment.
Yet it’s a potential signal of cervical changes pressing on nearby tissues.
Speaking up about this, even if it feels awkward, is crucial. Many women regret delaying because of hesitation.
4. Pelvic or Lower Back Pain
Persistent pain in the pelvis, lower abdomen, or back that doesn’t go away shouldn’t be ignored.
As cancer advances, it can affect nerves and surrounding areas, leading to chronic discomfort.
Think of it as your body’s gentle reminder to seek attention.

5. Persistent Fatigue and Weakness
Feeling exhausted all the time, even with adequate rest, isn’t just “part of life.”
It could relate to anemia from blood loss or your body responding to illness.
If fatigue lingers without explanation, pair it with other signs for a fuller picture.
6. Unexplained Weight Loss and Loss of Appetite
Shedding pounds without trying, especially alongside reduced appetite, can indicate metabolic changes.
Research links this to advanced stages where the body is under stress.
But that’s not all—combine it with other symptoms, and it’s a stronger prompt to act.
7. Leg Swelling or Pain
Swelling in one or both legs might occur if cancer affects blood flow or lymph nodes.
Often dismissed as fatigue-related, it’s more common in later stages.
8. The Most Overlooked Factor: Persistent High-Risk HPV Infection
Here’s the silent alarm many women miss: long-lasting infection with high-risk HPV types causes over 95% of cervical cancers, according to the World Health Organization.
You might have zero symptoms. That’s why this is the most under-recognized “sign”—there often isn’t one.
Regular Pap smears and HPV tests are essential to detect it early.

Risk Factors That Increase Your Chances
Certain factors can elevate risk. Here’s a quick overview:
- Persistent HPV infection: The primary cause.
- Smoking: Doubles the risk, as it weakens the immune system.
- Weakened immunity: From conditions like HIV.
- Multiple sexual partners: Increases HPV exposure.
- Early sexual activity or multiple births: Linked in studies.
- Long-term oral contraceptive use: Slight increase noted.
But lifestyle changes can help mitigate some risks.
How to Protect Yourself: Actionable Steps
Prevention and early detection are in your control. Start with these practical steps:
- Get vaccinated: The HPV vaccine is highly effective if given before exposure, ideally ages 9-26.
- Schedule regular screenings: Pap tests starting at 21, co-testing with HPV from 30. Follow your doctor’s guidelines.
- Practice safe sex: Use condoms and limit partners.
- Quit smoking: It significantly lowers risk.
- Monitor your body: Note changes in a journal and report them promptly.
- Talk to your doctor: If concerned, request an exam or test—no question is too small.
Small actions today add up to big protection tomorrow.
Conclusion: Listen to Your Body and Take Charge
Cervical cancer doesn’t have to be a frightening threat. With awareness of these signs, regular screenings, and preventive measures like vaccination, most cases can be prevented or managed effectively.
Your health journey is personal, but you’re not alone. By tuning into your body’s signals and prioritizing check-ups, you’re empowering yourself for a healthier future.
Start this week: Book that overdue screening or discuss HPV vaccination with your provider.
Frequently Asked Questions
At what age should I start cervical cancer screenings?
Most guidelines recommend starting Pap tests at age 21. From age 30, combining with HPV testing is often advised. Continue based on your doctor’s recommendations, even after menopause if not previously screened regularly.
Can the HPV vaccine help if I’m already sexually active?
Yes, it can still protect against HPV types you haven’t encountered. It’s most effective before exposure but beneficial up to age 26 (and sometimes beyond—discuss with your doctor).
Are these symptoms always cancer?
No—these can result from benign issues like infections or fibroids. However, persistent or unusual changes deserve evaluation to rule out serious causes.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider with any questions about your health or symptoms. Early detection through screenings is key, but individual risks vary.