Many hardworking adults in their 40s and 50s push through waves of unusual fatigue or mild discomfort, dismissing them as everyday stress, poor sleep, or just “getting older.” These subtle signals can actually indicate a silent heart attack—where heart damage occurs without the dramatic chest pain most people expect. The frustrating part? You might not realize it happened until much later, leaving your heart scarred and at higher risk for future problems.
But here’s the good news: becoming aware of these overlooked signs can empower you to take action early. Stick with me until the end—there’s one simple shift that could make all the difference in protecting your heart for years to come.

The Hidden Danger: Why Silent Heart Attacks Are So Common
A silent heart attack, also known as a silent myocardial infarction, happens when blood flow to part of your heart is blocked, causing damage—just without the intense symptoms.
According to recent data from the Centers for Disease Control and Prevention (CDC) and the American Heart Association (AHA), about 1 in 5 heart attacks in the United States are silent. That means the damage is done, but you may not notice it at the time.
These events are more likely in certain groups, including women, people with diabetes (due to potential nerve damage that masks pain), and older adults.
The real concern? Undetected damage can lead to scarring, weakened heart function, or a higher chance of a major heart event down the line.
Research shows that people who’ve had a silent heart attack face significantly increased risks compared to those who haven’t.
But that’s not all—many of these signs get brushed off as minor issues. Let’s change that.
What Exactly Is a Silent Heart Attack—and Why Does It Happen?
Imagine plaque building up quietly in your arteries over years. Suddenly, a blockage reduces oxygen to your heart muscle, causing injury.
Unlike a classic heart attack, there’s no crushing pain to alert you.
This “sneaky” nature explains why so many go unnoticed until a routine check or later complications reveal the truth.
Studies from sources like the Cleveland Clinic and Mayo Clinic highlight that symptoms, if present, are often mild and mistaken for something else.
The truth is, anyone with risk factors—like high blood pressure, high cholesterol, smoking, or family history—could experience this.
Here’s the interesting part: tuning in to your body’s quieter signals could help you catch it early.
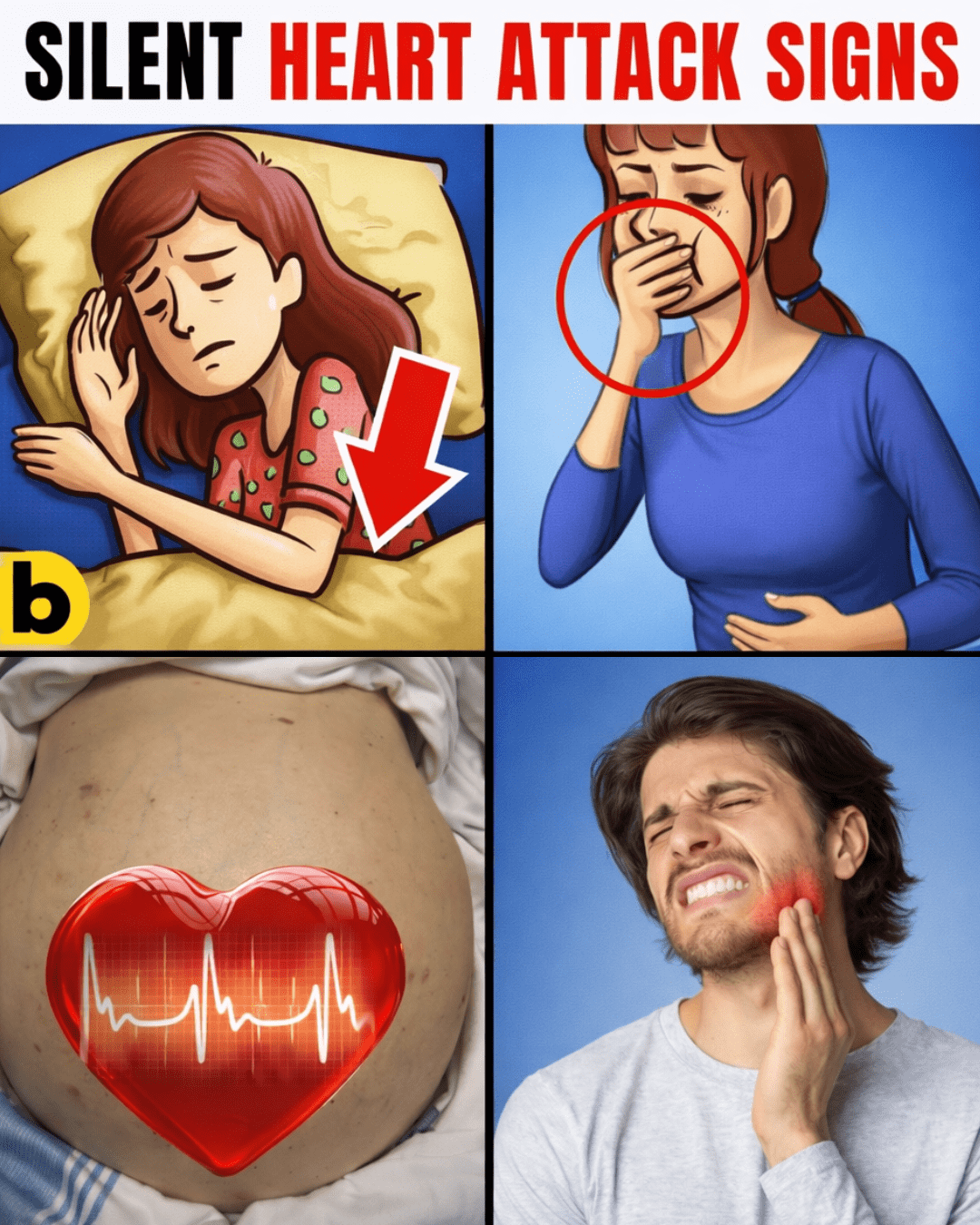
6 Subtle Signs You’re Probably Overlooking
Sign 1: Unusual Fatigue That Just Won’t Go Away
Feeling drained even after a full night’s sleep? This extreme tiredness can hit suddenly and linger, making daily tasks feel overwhelming.
It’s one of the most common subtle signs, especially in women, according to AHA insights.
Why? Reduced blood flow means your heart works harder to pump oxygen-rich blood, leaving you low on energy.
Many people blame stress or busy schedules—but if it’s persistent and unexplained, it deserves attention.

Sign 2: Mild Chest Discomfort Mistaken for Indigestion
A feeling of fullness, pressure, or burning in your chest after meals? It might seem like heartburn or acid reflux.
But this can actually signal reduced blood flow.
People with diabetes are especially prone to this, as nerve changes can dull sharper pain signals.
Research ties it to blocked arteries causing that “off” sensation.
Don’t just reach for antacids every time—note if it happens without obvious triggers.
Sign 3: Unexplained Cold Sweats or Clammy Feeling
Breaking out in a sweat without exertion or heat? This can occur even while resting.
Your body may release stress hormones in response to low oxygen, triggering sweats.
It’s a subtle clue often dismissed as anxiety or hormonal changes.
But combined with other signs, it could point to heart strain.

Sign 4: Flu-Like Symptoms That Linger
Ongoing mild nausea, muscle aches, or a general “under the weather” feeling for weeks?
These can stem from inflammation or reduced heart efficiency.
Many attribute it to a virus that “won’t quit.”
Yet studies link prolonged flu-like symptoms to underlying ischemia (reduced blood flow).
Sign 5: Sudden Bloating or Fluid Retention
Noticing swelling in your ankles, legs, or abdomen, or clothes feeling tighter?
This fluid buildup can happen when your heart isn’t pumping effectively, causing backup.
Often blamed on diet or salt intake.
But it’s a key sign of potential congestion from heart stress.
Sign 6: Discomfort in Jaw, Neck, Back, or Arms
Aching in your jaw, upper back, neck, or one/both arms—especially if it comes and goes?
Women often experience these atypical locations more than classic chest pain.
It happens when pain signals radiate from the heart.
Frequently mistaken for muscle strain or poor posture.
Here’s a quick comparison table of common dismissals vs. potential heart links:
| Ignored Sign | Common Dismissal | Potential Heart Link |
|---|---|---|
| Unusual fatigue | Stress or lack of sleep | Reduced oxygen delivery to body |
| Mild chest discomfort | Indigestion or heartburn | Pressure from blocked blood flow |
| Cold sweats | Anxiety or menopause | Body’s stress response to low oxygen |
| Flu-like symptoms | Lingering virus | Inflammation from reduced flow |
| Bloating/swelling | Diet or weight gain | Fluid backup from weaker pumping |
| Unusual pain (jaw/back/etc.) | Muscle strain or tension | Radiating signals from heart |
You’re now armed with all six—great job making it this far!

When to Seek Help: Diagnosis and Next Steps
If any signs persist for days or worsen with activity, don’t wait—see your doctor promptly.
Tests like an EKG, blood work for heart markers, or a stress test can reveal hidden damage.
Early detection matters immensely.
In emergencies (sudden severe symptoms), call 911 immediately.
Preventing Silent Heart Threats: Actionable Daily Habits
You can start protecting your heart today with these simple steps:
- Move more: Aim for 30 minutes of brisk walking most days to improve circulation.
- Eat heart-smart: Focus on fruits, vegetables, whole grains, lean proteins, and healthy fats like those in fish, nuts, and avocados.
- Manage stress: Try deep breathing, yoga, or short meditations daily.
- Monitor risks: Track blood pressure, cholesterol, and blood sugar regularly.
- Quit smoking: Seek support if needed—it’s one of the biggest wins for your heart.
- Stay hydrated and limit salt: Helps maintain healthy blood flow.
Here’s a simple habit timeline:
| Time Frame | Start With | Potential Benefits |
|---|---|---|
| Week 1-2 | Daily walks | Better blood flow and energy |
| Weeks 3-4 | Add nutrient-rich meals | Stabilize plaque and reduce inflammation |
| Month 2+ | Consistent routine + checkups | Lower overall risk factors |
Pro tip: Schedule annual checkups, especially if over 45 (men) or 55 (women), or with family history.
Imagine a Stronger Heart Tomorrow
Picture waking up energized, free from nagging discomfort, with more vitality for family and life.
By listening to these subtle signs and acting proactively, that’s within reach.
Thousands have turned things around—why not join them?
The “one thing” tying it all together? Your body is always communicating—start listening today.
Frequently Asked Questions
1. How common are silent heart attacks?
About 1 in 5 heart attacks are silent, per CDC and AHA data, meaning damage occurs without obvious symptoms.
2. Are silent heart attacks more dangerous than regular ones?
They can be, because delayed awareness leads to untreated damage, increasing risks like heart failure.
3. Who is at higher risk for a silent heart attack?
Women, people with diabetes, older adults, and those with risk factors like high blood pressure or smoking.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Symptoms can vary widely, and silent heart attacks may present differently based on individual factors. Always consult your healthcare provider for any concerns, especially if you have risk factors—seek emergency care if you suspect a heart event.