Many people experience heart attacks without the dramatic chest pain often shown in movies. In fact, about 1 in 5 heart attacks in the United States are silent, meaning the heart suffers damage but symptoms are so mild they’re easily dismissed as everyday issues like stress or indigestion. This can lead to undetected scarring that raises the risk of future problems, leaving you frustrated when something serious was happening all along without clear warning. But recognizing these overlooked signals early can empower you to seek help and protect your heart—stick around, because the real game-changer comes at the end.

The Hidden Danger of Silent Heart Attacks
Silent heart attacks, also known as silent myocardial infarctions, occur when blood flow to the heart is blocked, causing damage without obvious symptoms.
According to data from sources like the Centers for Disease Control and Prevention (CDC), around 805,000 heart attacks happen annually in the U.S., with approximately 1 in 5 being silent.
These events are more common in certain groups, including women, people with diabetes (due to potential nerve damage affecting pain perception), and older adults.
The frustration hits when mild discomfort gets brushed off as aging or a busy lifestyle—yet over time, this unnoticed damage can lead to heart weakening or higher risks down the line.
But here’s the encouraging part: Tuning in to your body’s subtle cues can make all the difference.
You’re already taking a positive step by reading this—keep going.

What Is a Silent Heart Attack, and Why Does It Go Unnoticed?
A silent heart attack happens just like a typical one: Plaque buildup in arteries leads to a blockage, reducing oxygen to the heart muscle and causing injury.
The difference? No intense pain or alarm bells.
Research from reputable sources, including the American Heart Association and Cleveland Clinic, shows these are sneakier because symptoms mimic common complaints.
They often affect women more atypically and people with diabetes, where nerve changes can dull sensations.
Think about that “off” feeling you’ve ignored lately—it might be worth noting.
The good news? Awareness and simple checks can reveal hidden issues early.
The 6 Subtle Signs You Shouldn’t Ignore
Let’s break down the most common subtle signs, backed by insights from medical experts.
Many people share stories of dismissing these until a routine check uncovered past damage.
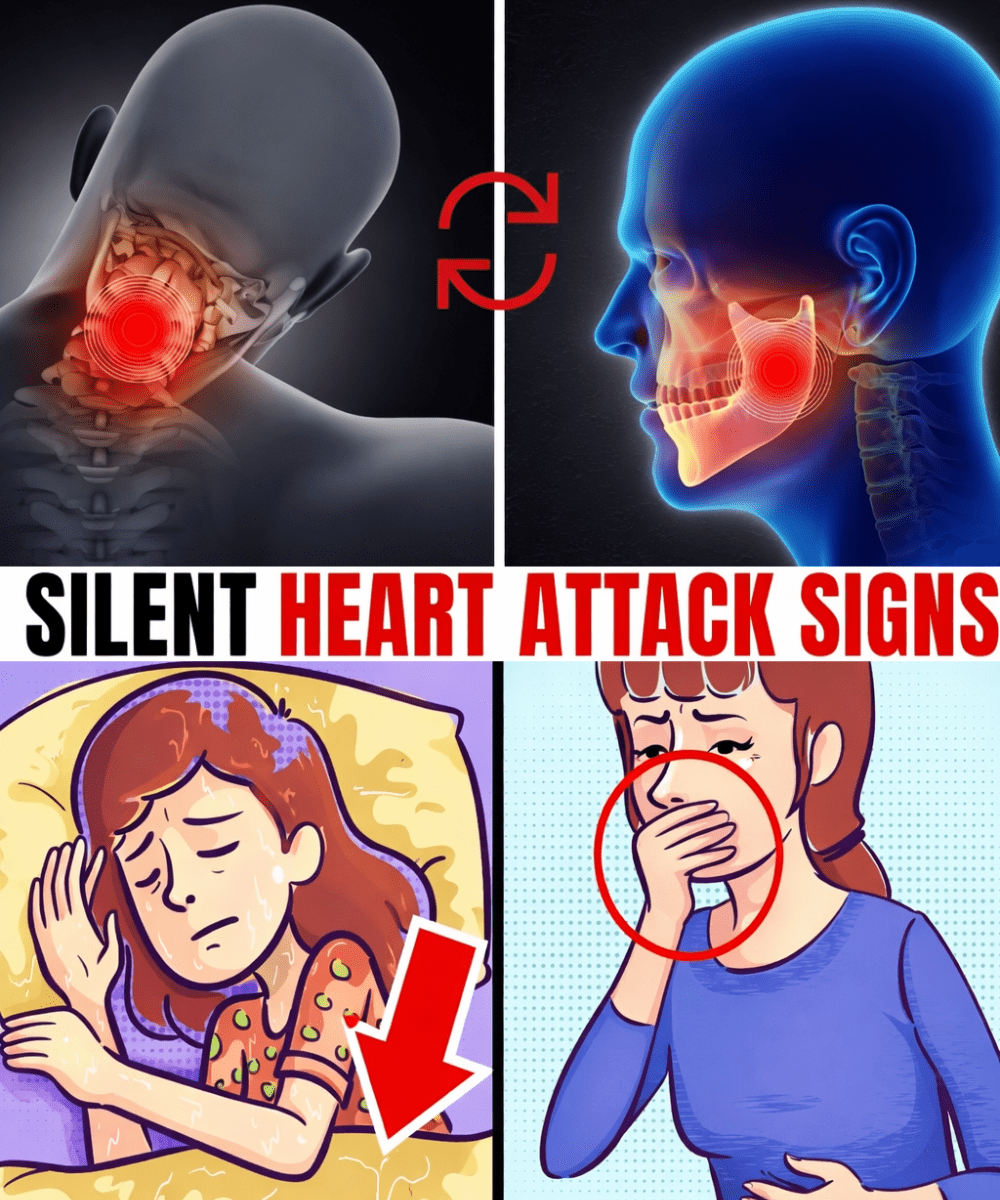
1. Unusual Fatigue That Won’t Go Away
Extreme tiredness that drains you, even after rest, tops the list—especially for women.
Studies highlight how reduced blood flow strains the heart, leading to less energy overall.
One common story: A busy professional chalked it up to long hours, only to learn later it signaled heart strain.
If persistent fatigue hits above a moderate level, it’s worth discussing with your doctor.
But fatigue isn’t the only deceiver…
2. Mild Discomfort Mistaken for Indigestion
That fullness or burning in your chest after meals? It might not be acid reflux.
Pressure from limited blood flow can feel just like digestive upset.
This is particularly common in people with diabetes, where symptoms may be milder.
Many reach for antacids, masking the issue—until tests show otherwise.
Self-check: If “indigestion” lingers without clear food triggers, pay attention.
Here’s where it gets even trickier…

3. Unexplained Cold Sweats at Rest
Breaking into sweats without exertion or heat can signal your body’s stress response to low oxygen.
This subtle sign often gets blamed on anxiety or hormonal changes.
Experts note it’s a key indicator to watch, especially if sudden.
Imagine catching this early—how empowering would that feel?
You’re halfway through the signs—great progress!
4. Lingering Flu-Like Symptoms
Feeling achy, nauseous, or under the weather for weeks?
Body-wide inflammation from reduced heart flow can mimic a virus.
Shortness of breath or mild cough might join in.
Research ties these to ongoing strain many overlook.
Quick tip: If symptoms drag on without improvement, consider a checkup.
Only two more to go…
5. Sudden Bloating or Fluid Retention
Swelling in ankles, legs, or a bloated feeling?
When the heart pumps less efficiently, fluid can back up.
This is often dismissed as diet or weight changes.
Tracking sudden shifts can clue you in.
6. Discomfort in Jaw, Neck, Back, or Arms
Pain radiating to unusual spots—like jaw ache or upper back tightness—without clear cause.
Women often experience this more than classic chest pressure.
It might feel like muscle strain from daily activities.
Congrats—you now know all six key signs!

Quick Comparison: Common Dismissals vs. Potential Links
To make it clearer, here’s a simple table of ignored signs and their possible heart connections:
| Ignored Sign | Common Dismissal | Potential Heart Link |
|---|---|---|
| Unusual fatigue | Stress or lack of sleep | Reduced oxygen delivery to the body |
| Mild chest discomfort | Indigestion or heartburn | Pressure from limited blood flow |
| Cold sweats | Anxiety or menopause | Body’s stress response to shortage |
| Flu-like symptoms | Lingering virus | Inflammation from reduced flow |
| Bloating/swelling | Diet or hormones | Fluid backup from weaker pumping |
| Unusual radiating pain | Muscle strain or poor posture | Signals from affected heart areas |
When to Seek Help and Next Steps
If any signs persist or combine, don’t wait—contact your healthcare provider.
Tests like an EKG, blood work, or imaging can detect past or ongoing issues.
Early action is key, as silent damage increases future risks.

Simple Habits to Protect Your Heart
Start small for big wins:
- Walk briskly daily: Aim for 30 minutes most days to improve circulation.
- Eat heart-friendly foods: Add fiber-rich veggies, fruits, omega-3s from fish or nuts.
- Manage stress: Try deep breathing or short walks.
- Monitor basics: Track blood pressure, cholesterol, and glucose if at risk.
- Quit smoking: Seek support if needed—it’s a game-changer.
| Timeline | Start With | Potential Benefits |
|---|---|---|
| Week 1-2 | Daily walks | Better blood flow |
| Weeks 3-4 | Nutrient-rich meals | Support artery health |
| Month 2+ | Consistent routine + checkups | Lower overall risk factors |
Pro tip: Schedule regular checkups, especially over age 45 or with family history.
Imagine a Stronger Heart Ahead
Picture waking energized, confident in your body’s signals, with more vitality for what matters.
Ignoring these can add risks, but listening and acting empowers you—thousands do it every day.
Your “one thing” to tie it all? Pay attention to changes and talk to your doctor openly.
Frequently Asked Questions
What makes silent heart attacks more common in women or people with diabetes?
Women often have atypical symptoms, while diabetes can affect nerve sensitivity, making pain less noticeable—per insights from Cleveland Clinic and similar sources.
Can a silent heart attack happen without any symptoms at all?
Yes, some have zero noticeable signs, only discovered later through tests.
How can I tell if past fatigue was a silent sign?
Persistent, unexplained tiredness warrants a checkup—your doctor can assess with simple tests.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Symptoms can vary widely, and silent heart attacks may present differently based on individual factors. Always consult your healthcare provider for any concerns, especially if you have risk factors, and seek immediate emergency care if you suspect a heart event.