Many people with pancreatic cancer experience subtle changes in their body for months—or even longer—before receiving a diagnosis. These signs are often brushed off as normal aging, stress, indigestion, or minor digestive issues. The result? Valuable time slips away as the disease progresses quietly.
What starts as occasional discomfort or unexplained tiredness can gradually build into a pattern that’s hard to ignore in hindsight. Research from leading organizations shows that pancreatic cancer is frequently found at advanced stages because its early signals are vague and nonspecific. But recognizing these patterns early doesn’t mean jumping to conclusions—it means knowing when to seek clarity from a doctor.
Stay with me, because by the end of this article, you’ll have a clear understanding of the most common warning signs, why they’re often missed, and the simple steps you can take today for greater peace of mind.

Why Pancreatic Cancer Is Often Diagnosed Late
Pancreatic cancer earns its “silent” reputation not because it lacks symptoms, but because those symptoms mimic everyday complaints. Studies indicate that only about 10-20% of cases are caught at an early, more treatable stage, with many diagnosed when the cancer has already spread.
Every year, countless adults experience ongoing abdominal discomfort, fatigue, or digestive changes—most turn out harmless. That’s the challenge: distinguishing “normal” from “pay attention.”
But here’s the key insight from clinical experience and population data: when multiple subtle signs appear together and persist, they deserve a closer look. The good news? Awareness and timely conversations with healthcare providers can make a real difference.
But that’s not all—let’s dive into the symptoms that research highlights as potential early indicators.
Symptom #1: Persistent Upper Abdominal Pain That Radiates to the Back
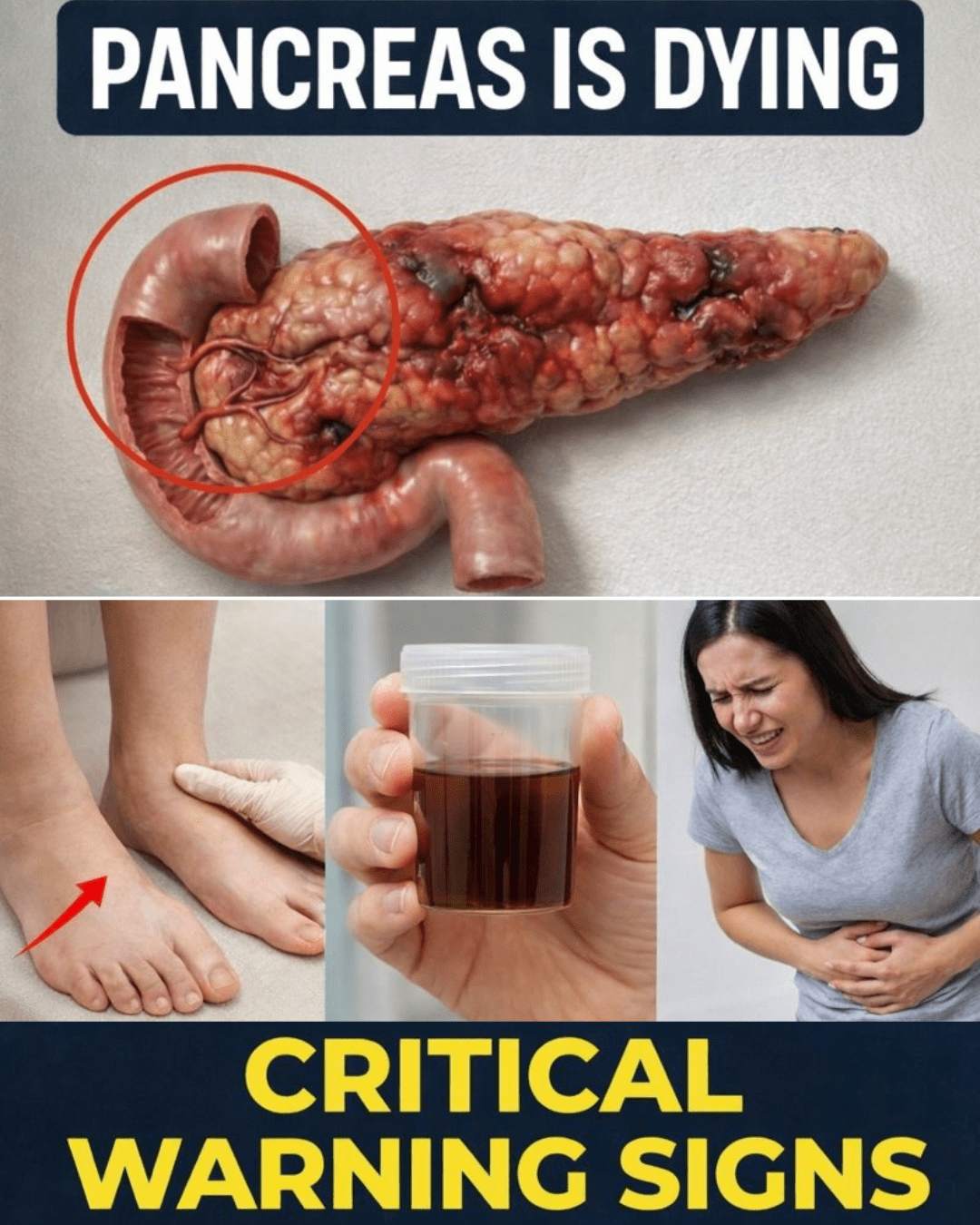
One of the most reported signs is a dull, nagging ache in the upper abdomen that spreads to the back. It may feel deeper than typical muscle strain and often worsens after eating or when lying down.
Many describe it as uncomfortable rather than sharp, which is why it’s easy to dismiss as posture-related or indigestion.
Self-check: Over the past month, have you noticed unexplained discomfort in your mid-back or upper belly that doesn’t fully resolve with rest or over-the-counter remedies?
This alone isn’t definitive, but persistence matters—especially when new or changing.
And pain is often just the starting point…

Symptom #2: Unintentional Weight Loss Without Trying
Losing 10 pounds or more without dieting, increasing exercise, or any obvious reason is a red flag that shouldn’t be ignored.
In pancreatic conditions, this can stem from poor nutrient absorption or metabolic shifts, sometimes before appetite noticeably drops.
Quick reflection: When did you last see an unexpected change on the scale?
When paired with other digestive or energy issues, unintentional weight loss prompts doctors to investigate further.
Here’s the twist: your appetite might still seem normal at first.
Symptom #3: Loss of Appetite or Feeling Full Too Quickly
You sit down to a meal you usually enjoy, but after a few bites, you feel oddly satisfied—or even turned off by food.
This early satiety happens when digestive signals get disrupted, leading to smaller portions over time and contributing to weight loss.
Mirror moment: Pushing away your plate halfway through a favorite dish isn’t just “being careful”—it can signal something deeper when ongoing.
But appetite shifts are often linked to broader digestive changes…

Symptom #4: Ongoing Indigestion, Bloating, or Changes in Bowel Habits
Frequent bloating, gas, nausea, or stools that float, look greasy, or smell unusually foul can point to issues with fat digestion.
These occur when the pancreas isn’t producing or releasing enough enzymes effectively.
Most people blame food sensitivities or stress—but when these persist despite changes in diet, it’s worth noting.
Self-assessment: Do you experience digestive discomfort that doesn’t tie clearly to specific meals or triggers?
And now we reach a symptom that’s hard to miss once it appears.
Symptom #5: Yellowing of the Skin or Eyes (Jaundice)
A yellowish tint to the skin or the whites of the eyes often signals bile flow blockage. It may come with dark urine, pale stools, and itchy skin.
Jaundice tends to prompt quicker medical attention because it’s visible.
STOP for a second: Have you noticed unusually dark urine lately, even when drinking plenty of water?
This symptom always warrants prompt evaluation, no matter the suspected cause.
But sometimes the itch arrives before the color change…

Symptom #6: Persistent Itching Without an Obvious Rash
Widespread itching that doesn’t respond to lotions, antihistamines, or typical remedies can feel frustratingly mysterious.
When related to bile buildup, it affects the whole body and intensifies over time.
Self-check: On a scale of 1-10, how bothersome has any unexplained itching been recently?
This becomes more concerning alongside digestive or urine/stool changes.
Next up is a sign many attribute to modern life.
Symptom #7: New or Worsening Fatigue That Doesn’t Improve With Rest
We’re not talking about end-of-day tiredness—we mean a heavy, persistent exhaustion that lingers even after sleep or rest.
It can interfere with daily routines and feel different from “normal” busy-life fatigue.
Picture this: Mid-afternoon crashes that leave you struggling, even on lighter days.
When combined with weight loss or pain, patterned fatigue adds to the bigger picture.
And sometimes, blood sugar plays a surprising role.
Symptom #8: New-Onset Diabetes or Unexpected Blood Sugar Changes
In some adults—especially over 50—newly developed diabetes or sudden blood sugar fluctuations (particularly with weight loss) have been linked to pancreatic issues in research.
This doesn’t mean every case of diabetes signals cancer, but the association is documented enough to warrant attention when other signs are present.
Quick question: Have your blood sugar levels shifted noticeably in the past year without a clear explanation?
Halfway through—great job staying engaged. You’re already more aware than most.
Symptom #9: Changes in Stool Color, Consistency, or Frequency
Pale, clay-colored, greasy, or hard-to-flush stools often indicate malabsorption of fats.
Foul odor or floating stools are common complaints people hesitate to mention.
Self-assessment: Have your bowel movements changed in multiple ways simultaneously—like color plus texture?
These shifts alongside appetite or weight changes help connect the dots.
And finally, the symptom that’s hardest to quantify but incredibly common…
Symptom #10: A Vague Gut Feeling That “Something Isn’t Right”
Many people later recall a prolonged sense of unease—small things not adding up, energy off, digestion quirky—before a diagnosis.
This isn’t imagination; it’s your body’s way of signaling pattern disruption.
You’re not overreacting by noticing. You’re being attentive.
Common Symptoms vs. Often-Assumed Causes (Quick Comparison)
Here’s a simple breakdown to help spot when a symptom deserves a second look:
- Symptom: Upper abdominal/back pain
Common assumption: Muscle strain or poor posture
Why reconsider: Persistent and unexplained, especially if worsening after meals - Symptom: Unintentional weight loss
Common assumption: Stress, busy schedule, or “better eating”
Why reconsider: No intentional changes + other signs - Symptom: Ongoing indigestion/bloating
Common assumption: Food intolerance or aging
Why reconsider: Doesn’t resolve with diet tweaks - Symptom: Fatigue
Common assumption: Lack of sleep or normal life demands
Why reconsider: Doesn’t improve with rest + patterned - Symptom: Jaundice/itching
Common assumption: Dehydration or allergy
Why reconsider: Requires medical evaluation promptly
What To Do If You Notice Multiple Symptoms
You don’t need to panic—you need to act thoughtfully. Here’s a simple step-by-step plan:
- Track your symptoms for 1-2 weeks: Note when they occur, severity (1-10 scale), and any triggers.
- Record basics: Recent weight changes, stool/urine observations, energy levels, appetite.
- Schedule a visit: Share your notes clearly with your doctor—mention patterns, not just one symptom.
- Ask questions: “What tests might help rule things out?” or “Could this be related to my pancreas?”
- Follow through: Early evaluation often brings reassurance or timely next steps.
Bookmark this page. Share it with loved ones. Awareness is one of the most powerful tools we have.
The One Thing That Ties It All Together
Pancreatic cancer isn’t defined by one dramatic symptom—it’s the combination and persistence that matters. Recognizing patterns early empowers you to seek information rather than live with uncertainty.
Imagine 30 days from now: You’ve paid attention, asked questions, and gained clarity. That’s the real win—knowledge and peace of mind.
Frequently Asked Questions (FAQ)
What are the earliest symptoms of pancreatic cancer?
Early signs are often vague, including fatigue, mild abdominal discomfort, appetite changes, and unintentional weight loss. Many mimic common issues, which is why patterns matter more than single symptoms.
Can pancreatic cancer cause diabetes?
Yes, in some cases, new-onset diabetes (especially in adults over 50 with weight loss or abdominal pain) has been associated with pancreatic cancer in research. However, most diabetes cases have other causes—consult a doctor for personalized assessment.
How is pancreatic cancer usually found?
It’s often discovered after symptoms prompt imaging tests like CT scans, ultrasounds, or blood work. Early detection is challenging, but discussing persistent symptoms with a healthcare provider increases the chance of timely evaluation.
This article is for informational purposes only and is not a substitute for professional medical advice. Always consult a qualified healthcare provider for any health concerns or symptoms you may be experiencing.